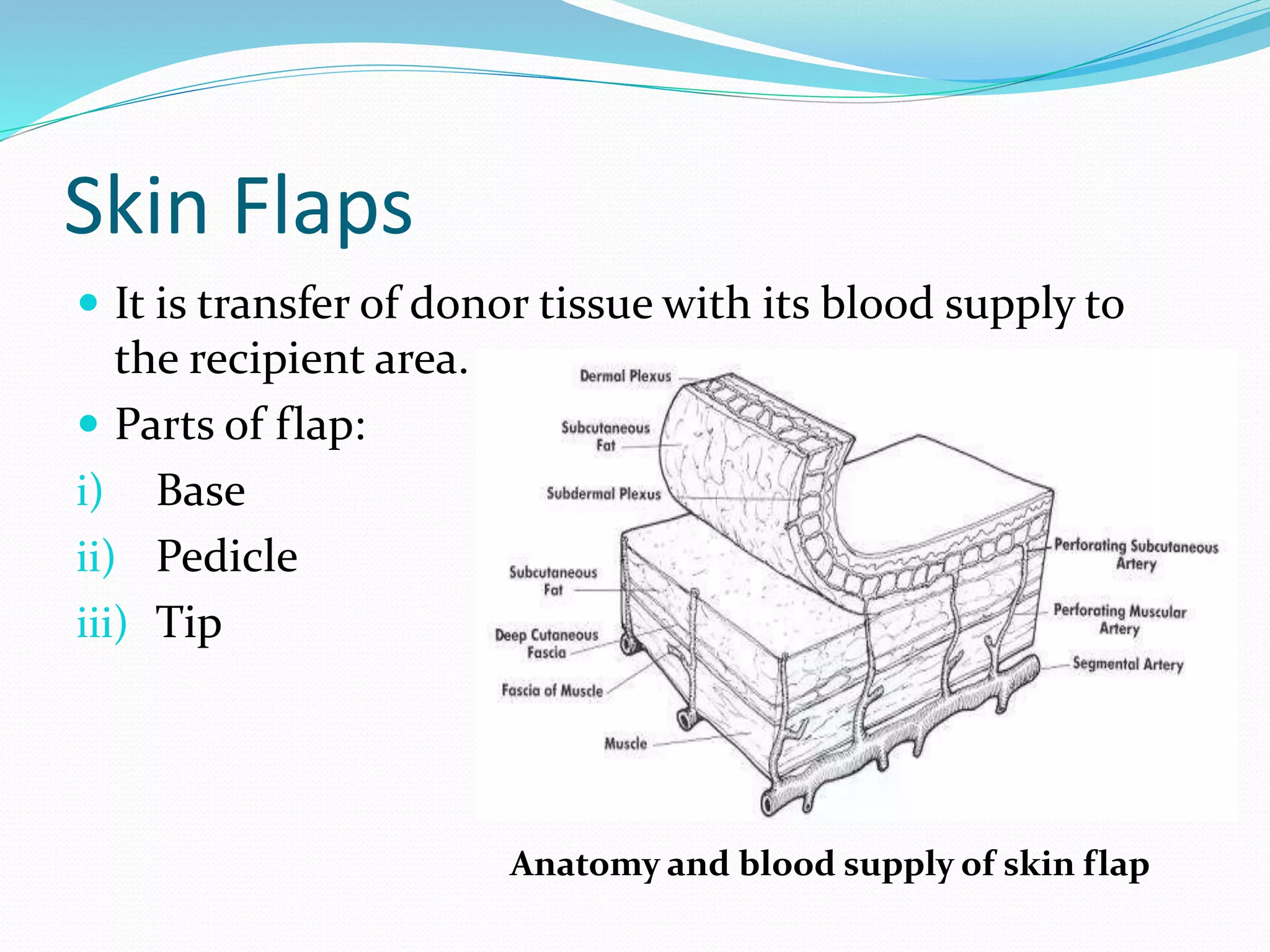
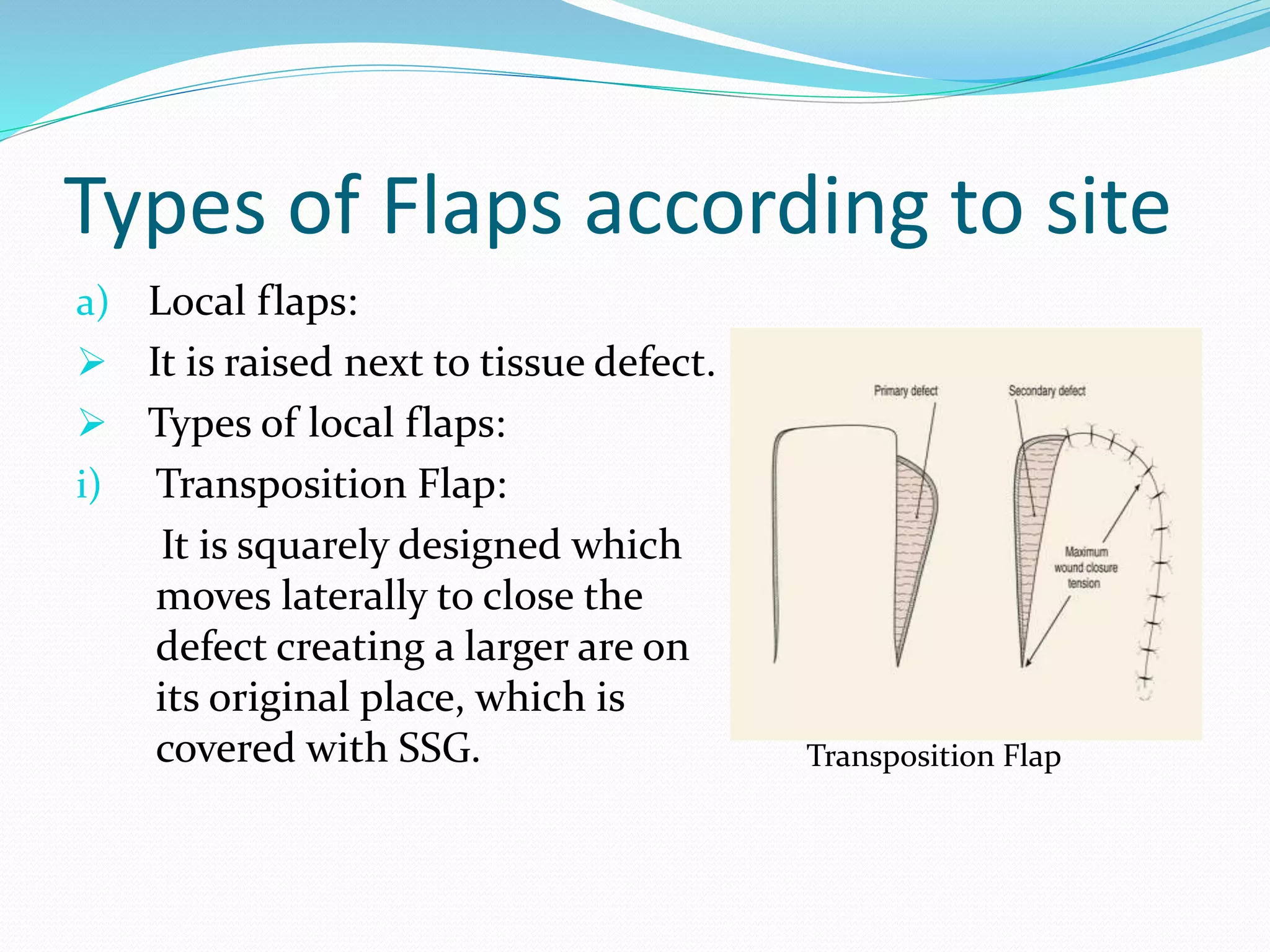
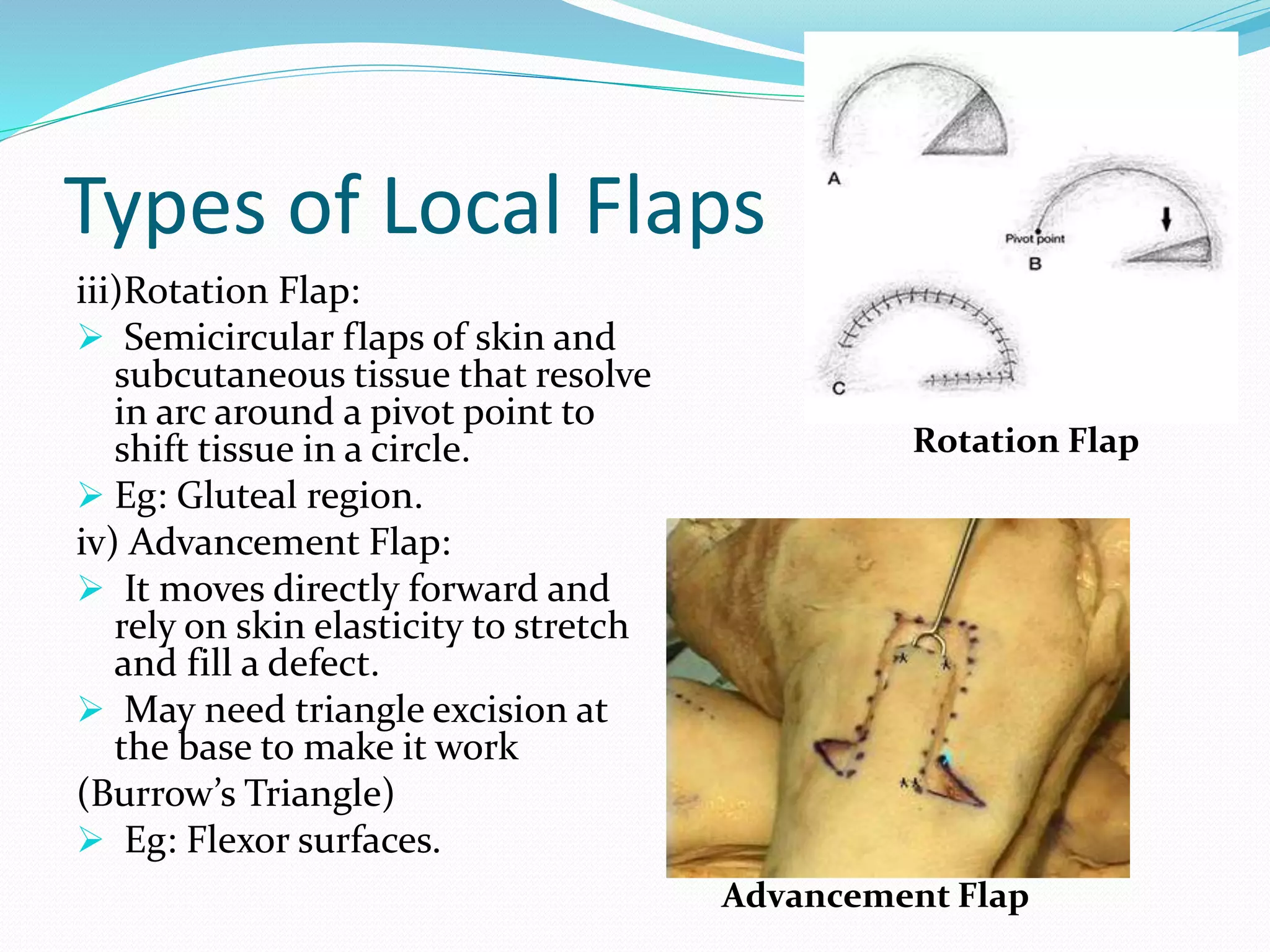
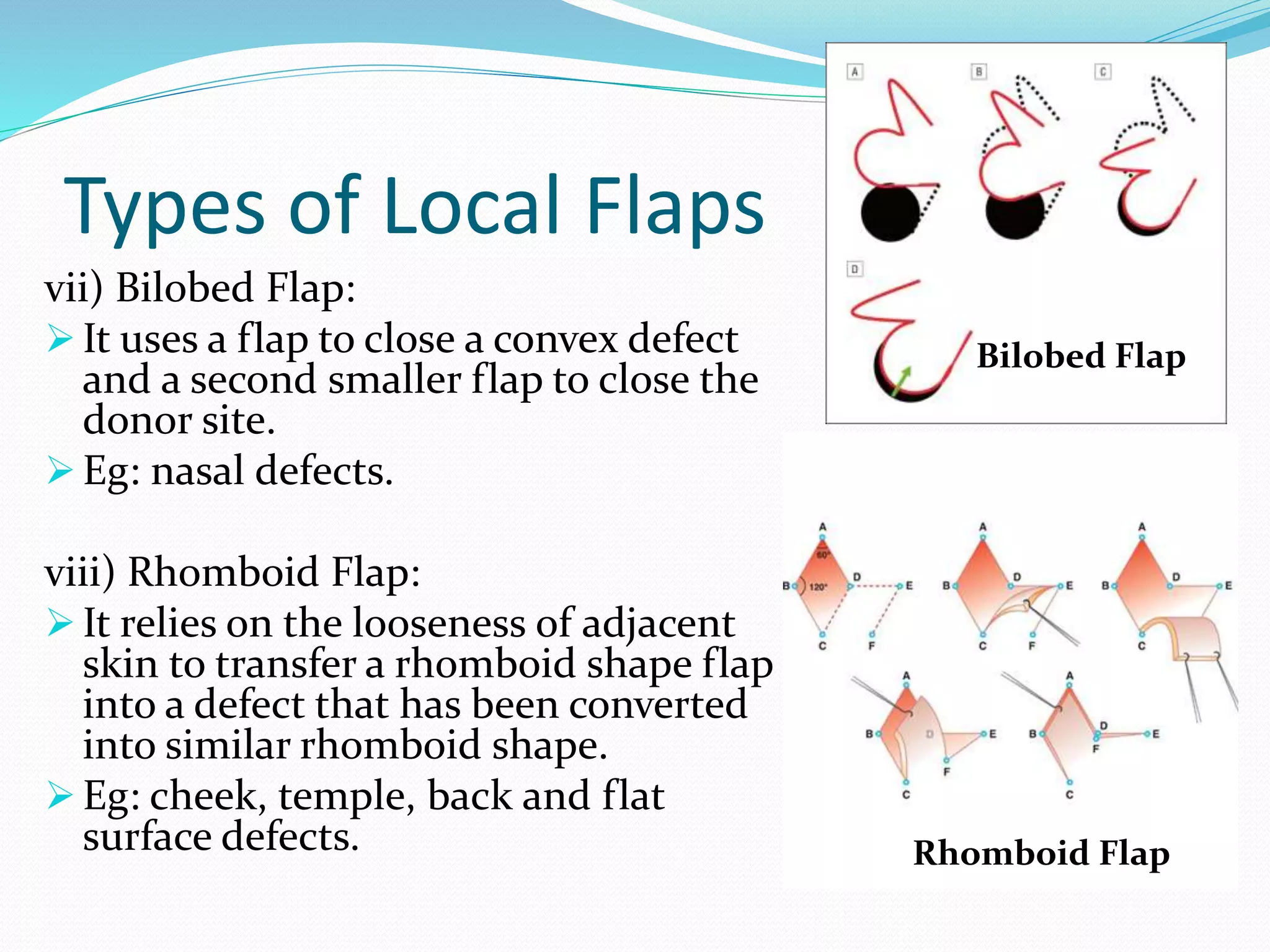
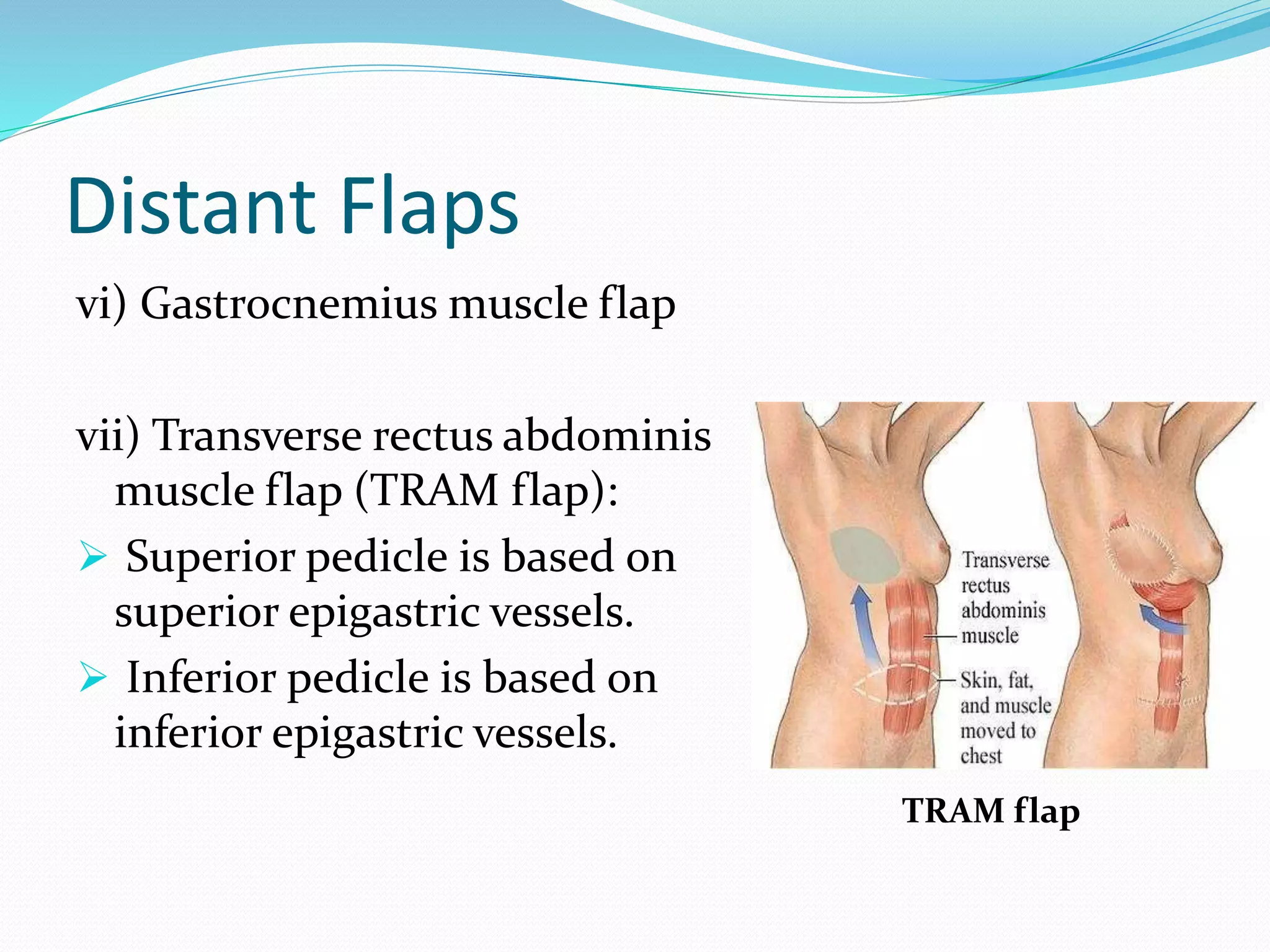
The document discusses the anatomy and types of skin grafts and skin flaps. It describes that skin has two layers, the epidermis and dermis. There are two types of skin grafts - partial thickness grafts which remove some dermis and full thickness grafts which remove the full dermis. Skin flaps differ in that they maintain the blood supply of the transferred tissue. Local flaps use nearby tissue while distant flaps require long pedicles. The techniques, indications, and advantages/disadvantages of various skin grafts and flaps are outlined.