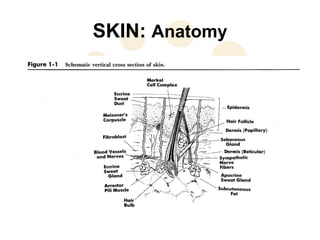
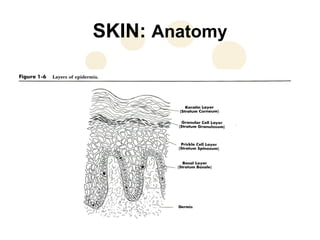
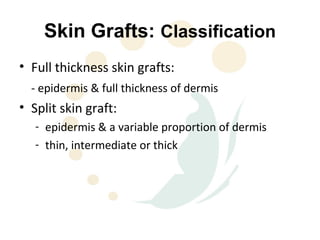
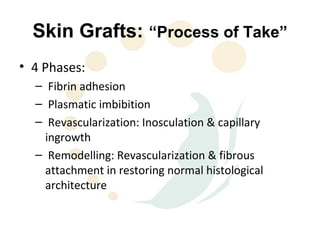
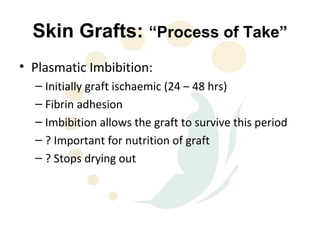
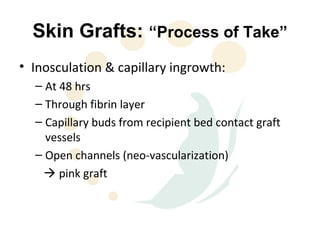
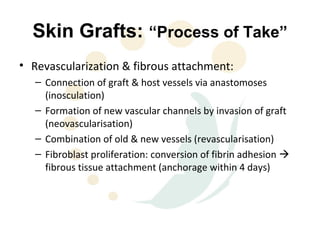
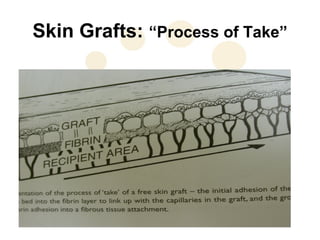
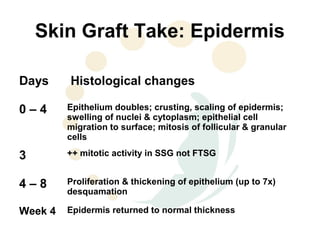
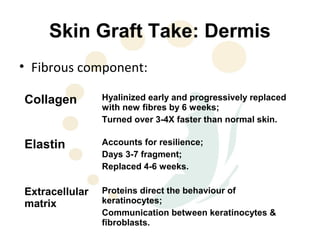
This document discusses the physiology and process of skin grafts. It describes the layers of skin - epidermis and dermis - and their functions. It explains the classification of different types of skin grafts including full thickness and split thickness grafts. The document then outlines the four phases of "take" that a skin graft undergoes as it revascularizes and attaches to the recipient bed. It provides details on the histological and structural changes that occur in both the epidermis and dermis as a graft heals over time. Factors that influence graft survival and potential causes of graft failure are also summarized.