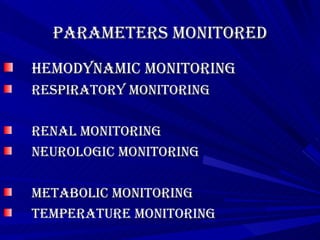
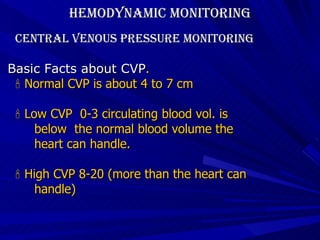
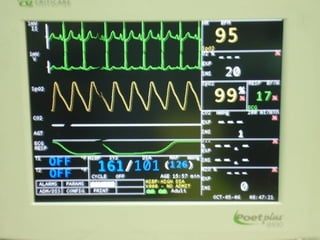
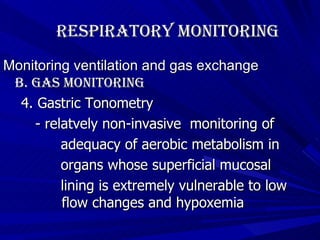
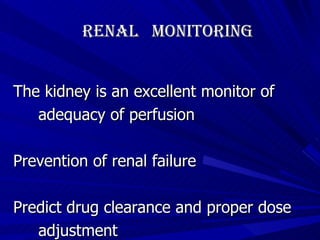
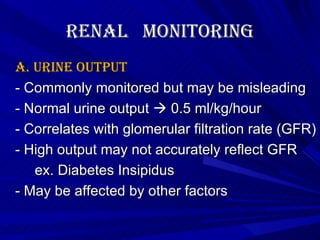
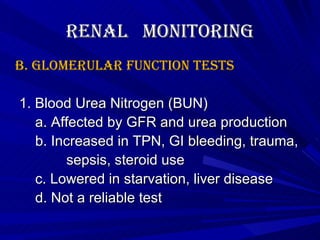
The document discusses various parameters that are monitored during physiologic monitoring, including hemodynamic monitoring (arterial and central venous catheterization), respiratory monitoring (ventilation and gas exchange), renal monitoring (urine output and glomerular function tests), and neurologic and metabolic monitoring. Key details provided include normal values, indications for monitoring, techniques, and potential complications.