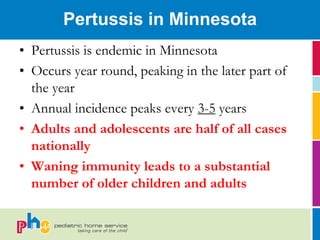
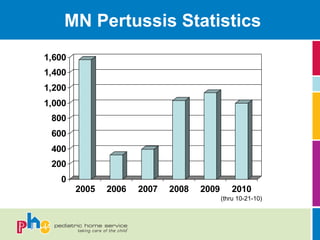
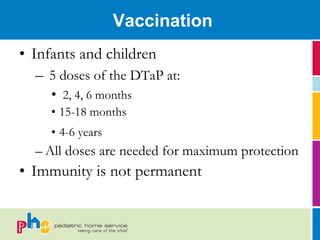
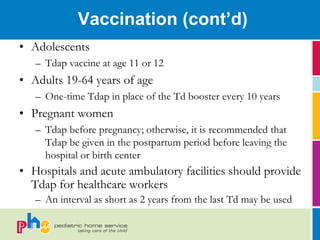
The document outlines the transmission, clinical features, treatment, vaccination, and prevention strategies for pertussis (whooping cough) in Minnesota, emphasizing its endemic nature and peak incidence patterns. It provides vaccination schedules for infants, children, adolescents, and adults, and highlights the importance of immunization for healthcare workers, particularly those caring for infants. Recommendations for exposure scenarios and infection control measures are also discussed, including the use of masks and antibiotic prophylaxis.