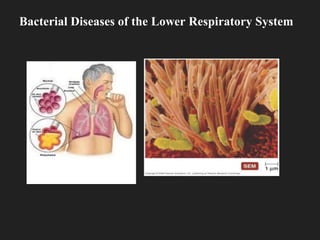
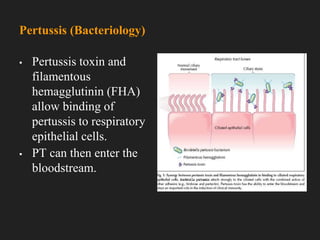
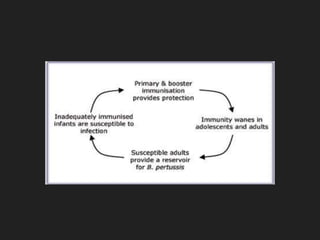
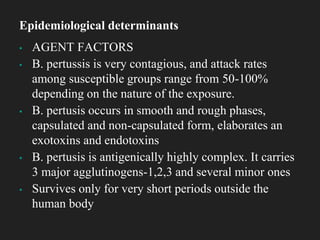
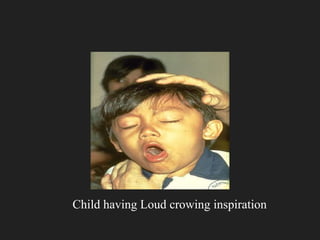
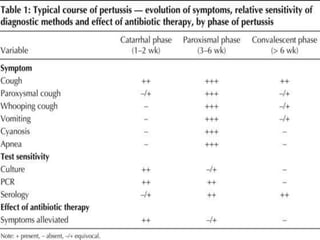
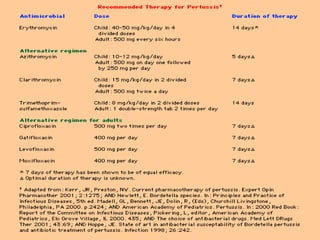
Whooping cough, or pertussis, is an acute infectious disease primarily affecting young children and caused by the bacterium Bordetella pertussis, which is highly contagious. The disease progresses through three stages: catarrhal, paroxysmal, and convalescent, with the characteristic 'whoop' often starting in the paroxysmal phase. Prevention includes vaccination, good hygiene practices, and antibiotics to interrupt transmission and treat symptomatic patients.