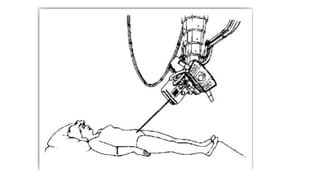
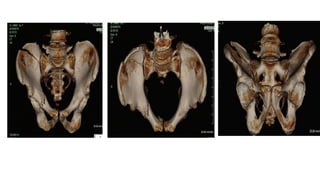
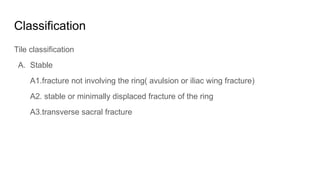
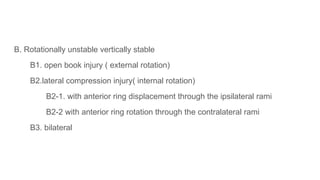
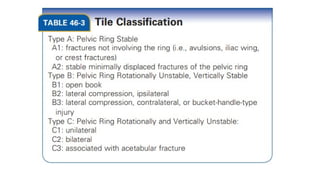
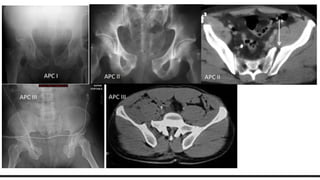
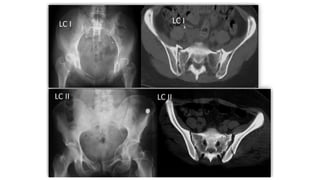
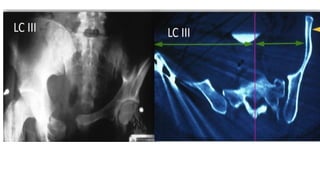
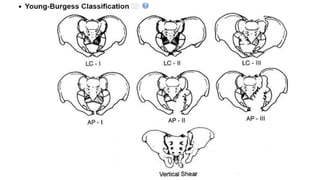
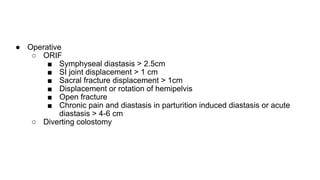
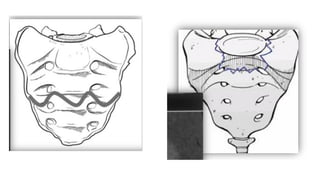
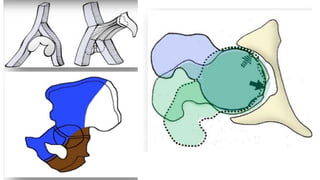
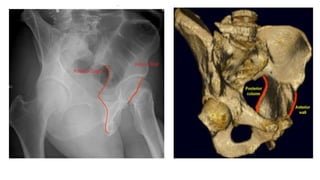
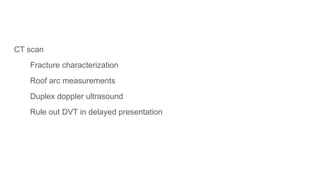
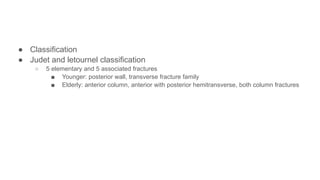
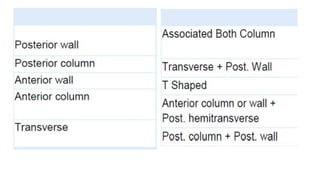
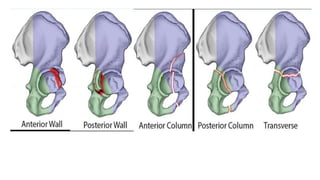
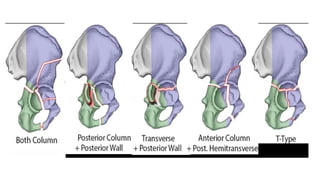
Pelvic fractures predominantly affect individuals aged 18 to 45, with a significant portion of cases in geriatrics and high morbidity and mortality rates due to associated injuries. The document discusses the mechanisms of injury, classifications of fractures, initial assessment and management protocols, as well as treatment options ranging from non-operative care to surgical interventions. It also outlines the anatomical considerations, diagnostic imaging techniques, and the complexity associated with pelvic and acetabular fractures.