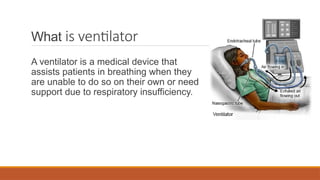
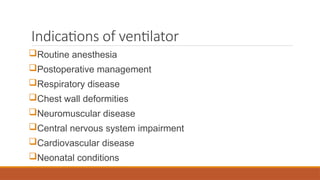
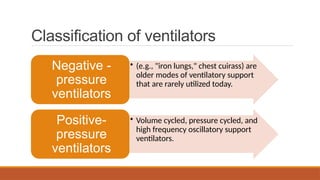
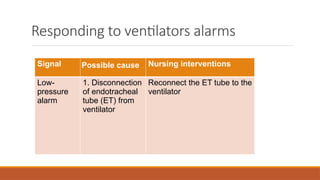
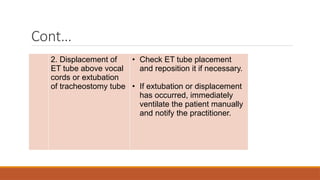
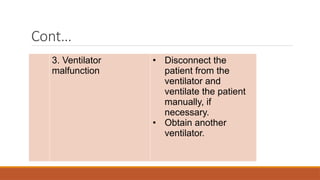
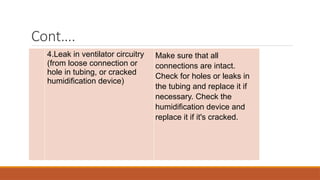
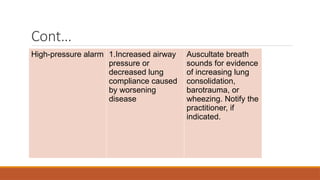
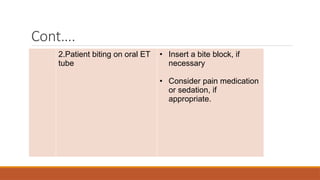
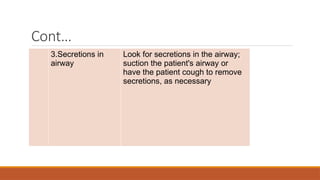
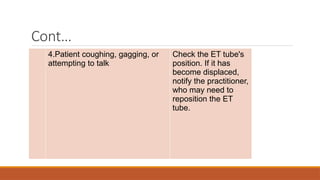
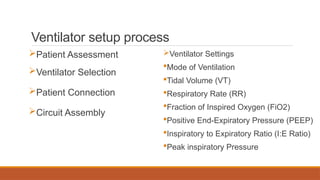
This document provides an overview of ventilator setup and management, detailing the purpose and classifications of ventilators, as well as their indications and settings. It discusses the techniques for invasive and non-invasive ventilation, common modes, types of alarms, and proper procedures for patient assessment, connection, and monitoring. Comprehensive training and expertise are emphasized as essential for healthcare professionals involved in ventilator management.