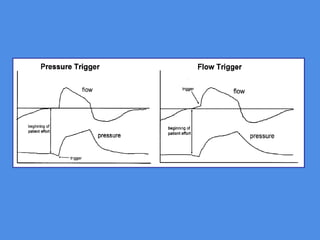
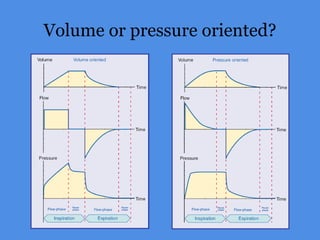
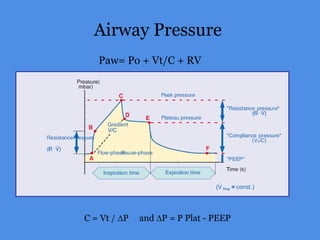
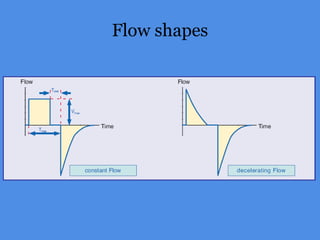
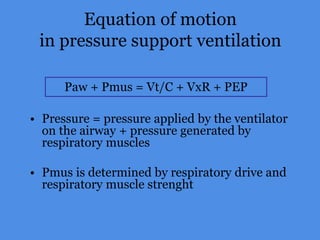
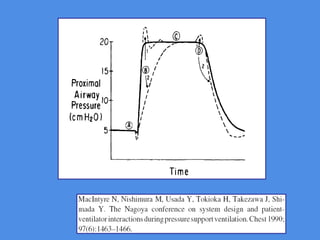
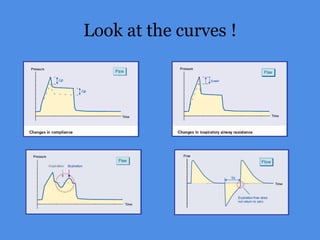
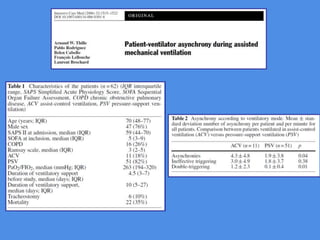
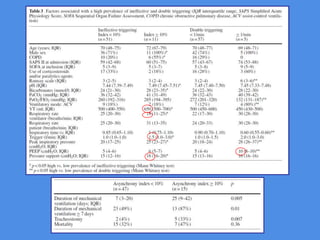
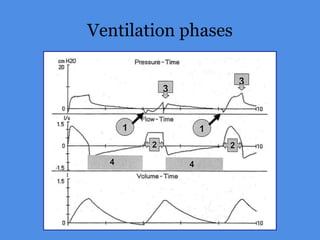
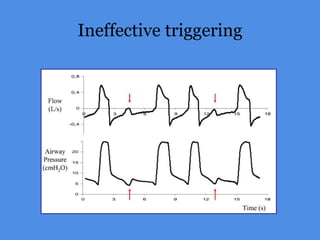
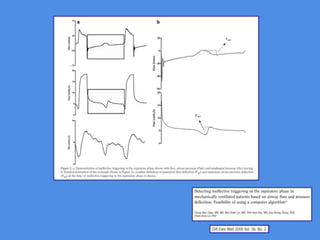
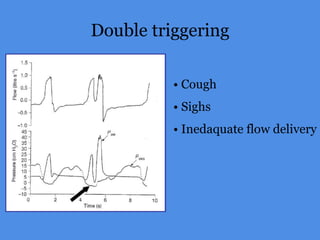
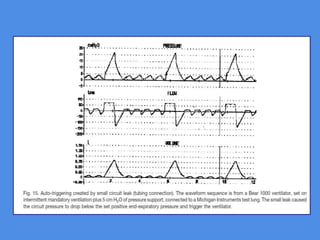
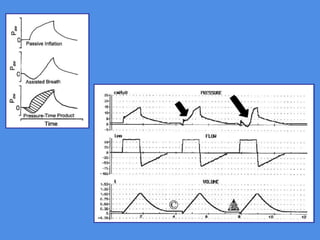
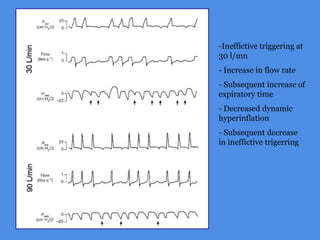
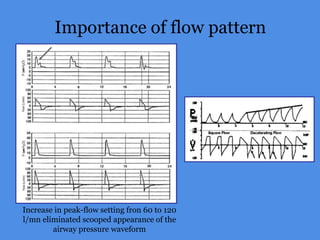
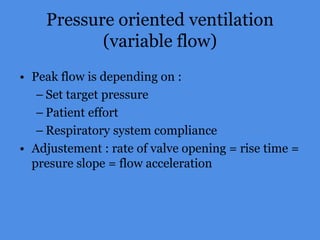
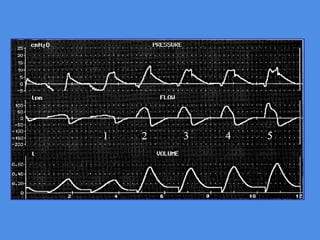
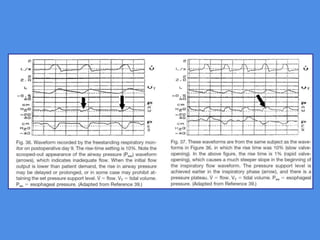
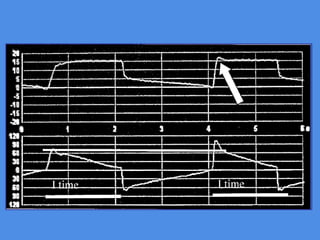
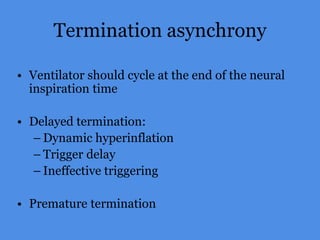
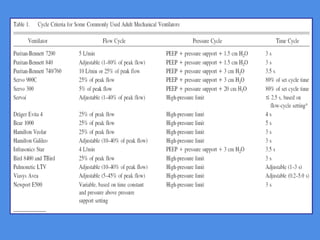
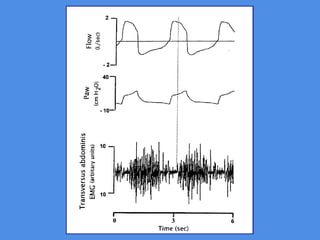
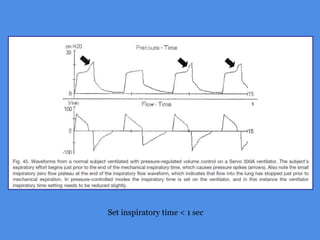
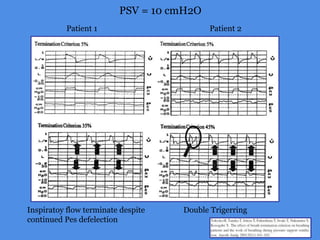
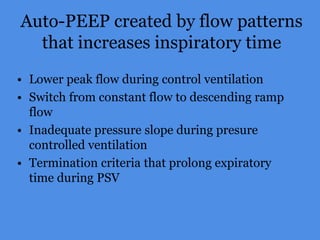
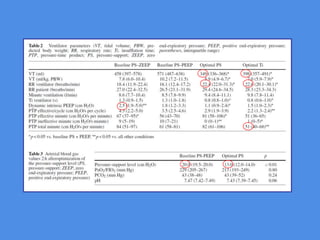
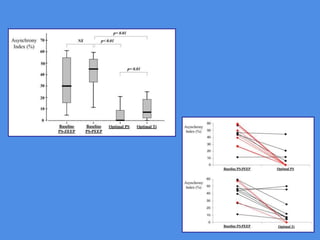
This document discusses patient-ventilator asynchrony, which occurs when there is a mismatch between the patient's respiratory effort and the ventilator's breathing cycles. It describes different types of asynchrony that can occur during triggering, cycling, flow delivery, and expiration. The key factors that determine inspiratory flow during pressure support ventilation are also examined. Close monitoring of pressure and flow waveforms is emphasized to identify asynchrony and adjust ventilator settings appropriately to reduce the patient's work of breathing.