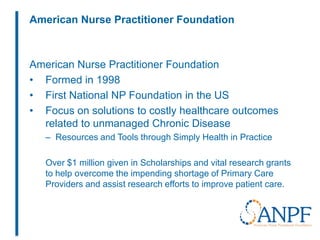
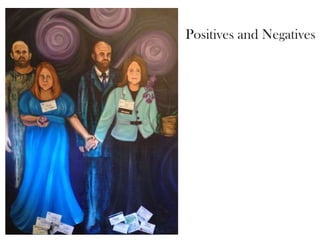
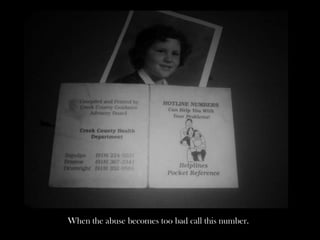
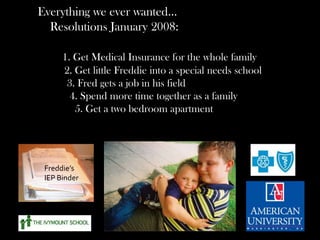
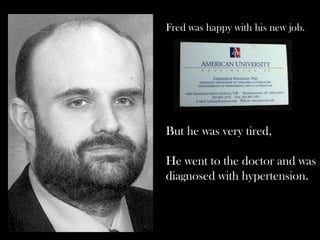
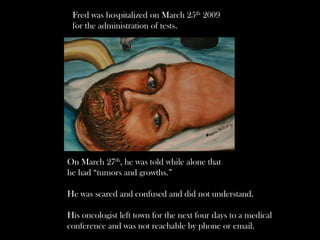
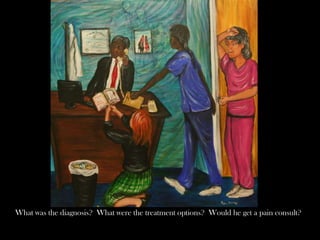
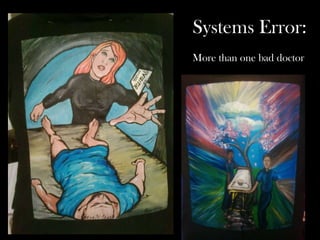
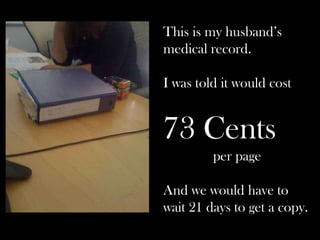
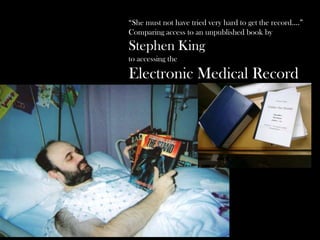
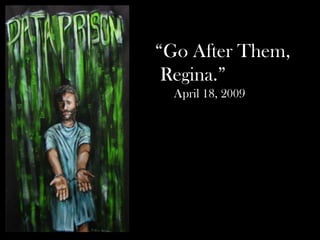
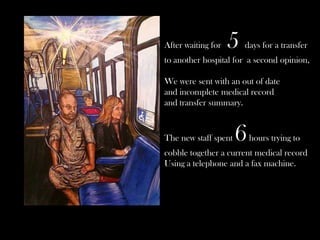
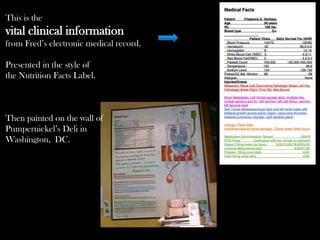
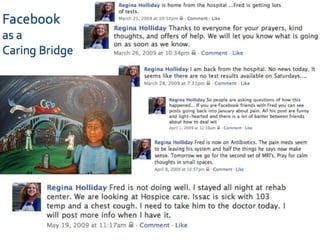
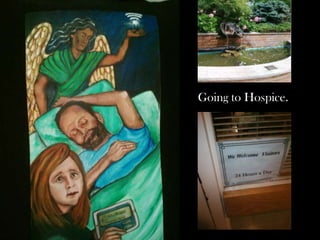
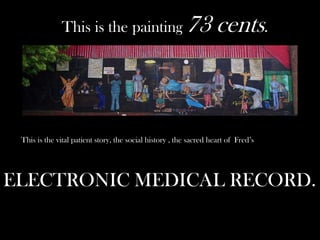
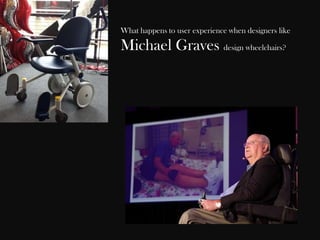
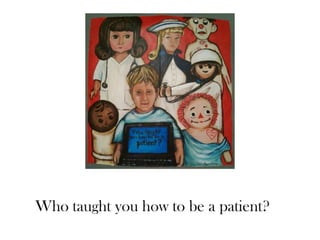
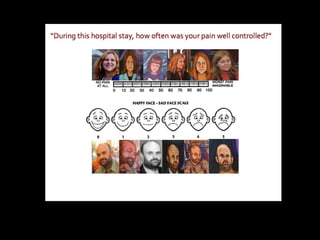
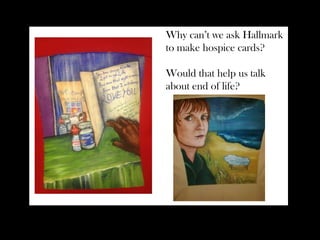
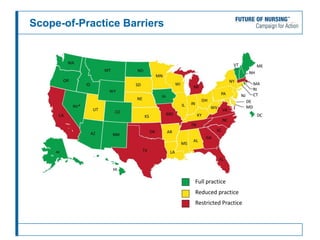
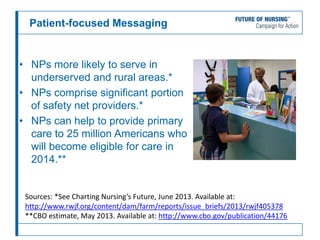
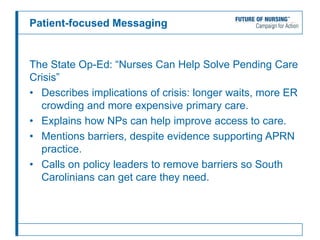
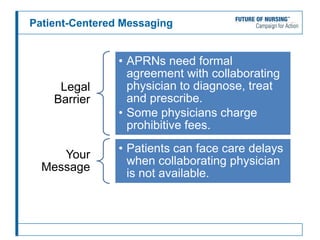
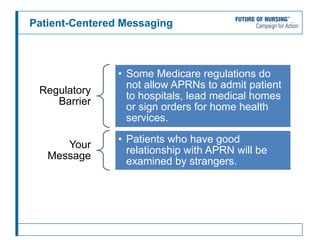
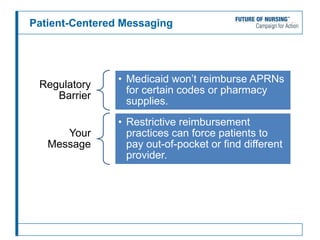
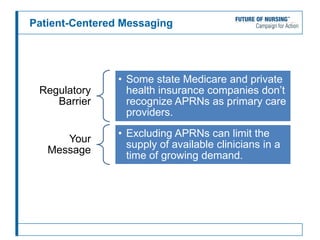
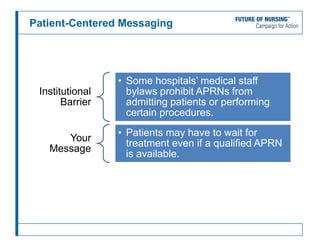
This webinar discusses patient advocacy and the role of healthcare providers and patients in creating legislative change. The speakers are Regina Holliday, a patient advocate and caregiver, and Susan Hassmiller, Senior Advisor for Nursing at the Robert Wood Johnson Foundation. Regina discusses the perspective of patients and caregivers, focusing on small details. Susan then discusses barriers to nurse practitioners' scope of practice and how to focus advocacy messaging on patients and their needs. The webinar aims to link advocacy messages to patient-centered focus.