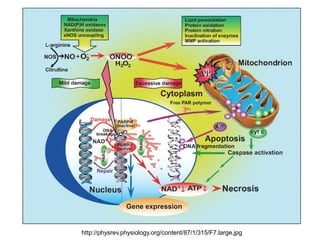
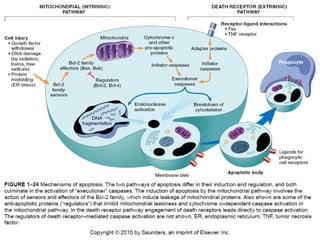
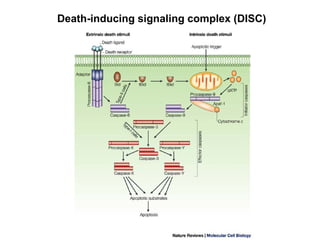
Cellular injury and cell death can occur through necrosis or apoptosis. Necrosis is unregulated cell death due to external factors like hypoxia or toxins. It is characterized by cellular swelling, membrane rupture, and inflammatory responses. Apoptosis is regulated cell death that occurs normally or in response to DNA damage. The cell shrinks and fragments into membrane-bound vesicles that are phagocytosed without inflammation. Both can result from ATP depletion, calcium flux, reactive oxygen species, or endoplasmic reticulum stress. The pattern of necrosis in tissue provides clues to the underlying cause, such as coagulative necrosis from ischemia.



























![Energy depletion
• Inhibition of oxidative phosphorylation
• [ATP] decreases
• Small changes, 5 - 10%, are sufficient to limit the
Na/K-ATPase and Ca/Mg ATPase
• Glycolytic capacity (glycogen stores) protects
from ATP depletion but leads to acidification
– Plasma and ER membranes swell
– Enzyme kinetics change; proteins begin to denature
– Chromatin clumps
• Denatured proteins either coagulate resulting in
necrosis or bind HSPs triggering apoptosis](https://image.slidesharecdn.com/patansb-221214194754-6fa4cd3e/85/Cell-death-pptx-33-320.jpg)

![Intracellular, cytosolic [Ca++] as
many as 4 orders of magnitude
lower than extracellular or
organellar (ER, SR, Mt)
Mitochondrial damage and ER
swelling releases Ca++ to
cytosol
Hydrolytic enzymes activated
Apoptosis may be activated
Necrosis occurs
Calcium Flux](https://image.slidesharecdn.com/patansb-221214194754-6fa4cd3e/85/Cell-death-pptx-35-320.jpg)