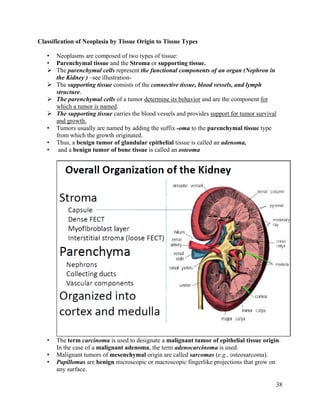
Cancer results from abnormal cell growth and differentiation. The four main steps in carcinogenesis are initiation, promotion, progression, and metastasis. Initiation involves DNA damage from factors like chemicals, radiation, or viruses. Promotion enhances the growth of mutated cells through exposure to factors like hormones or food additives. Progression refers to further growth and spread within the tissue. Metastasis is the spread of cancer to other organs. Genetic mutations in oncogenes, tumor suppressor genes, and DNA repair genes can drive uncontrolled cell growth. Cancer manifests through local effects on tissues and systemic effects like fatigue, weight loss, and abnormal hormone production. Tumor markers are substances released by cancer cells or in response to cancer that can