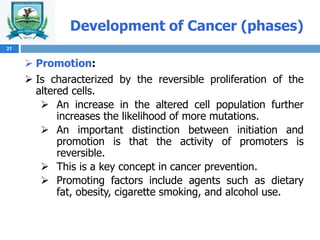
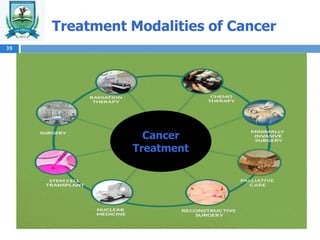
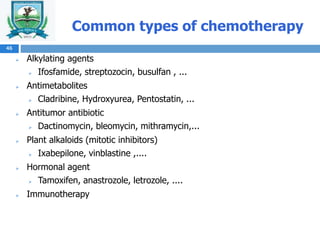
This document provides information on the assessment and management of cancer patients. It begins with learning objectives related to describing cancer incidence and mortality rates, the biology and stages of cancer development, and the nurse's role in cancer prevention, detection, diagnosis, and treatment. It then covers definitions of cancer, the origins and types of cancer cells, the biology of cancer development including defective cell proliferation and differentiation. The document discusses cancer staging and classification systems including TNM and the stages of cancer development. It also outlines common signs and symptoms of cancer, diagnostic tests, and the main goals and treatment modalities of cancer including surgery, radiation therapy, chemotherapy, targeted therapy, palliative care, nuclear medicine, and interventional radiology.