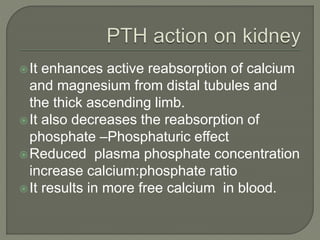
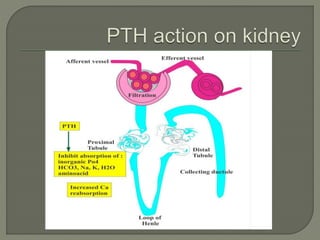
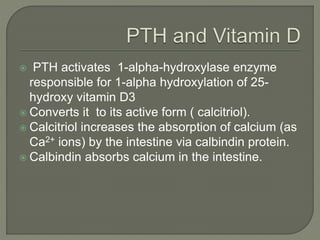
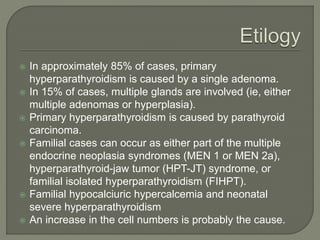
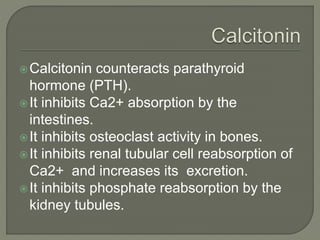
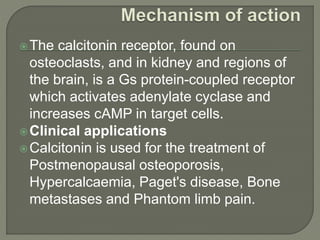
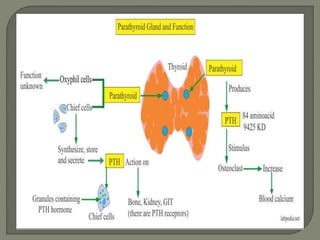
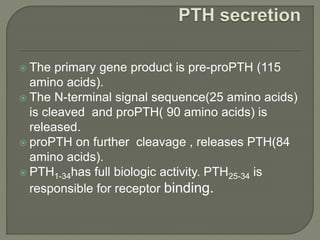
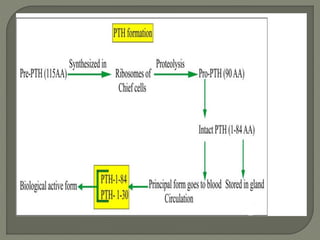
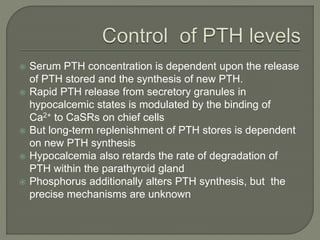
This document discusses the functions and regulation of parathyroid hormone (PTH), detailing its structure, secretion mechanisms, and implications in various disorders like primary hyperparathyroidism. PTH plays a crucial role in calcium homeostasis, stimulating bone resorption and affecting kidney function, while its secretion is primarily regulated by serum calcium levels through negative feedback. It also touches on the clinical manifestations of PTH-related conditions and treatment approaches, including the use of calcitonin.
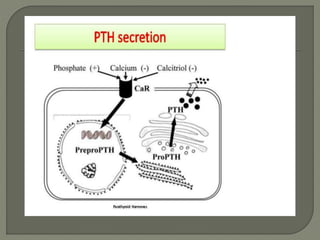
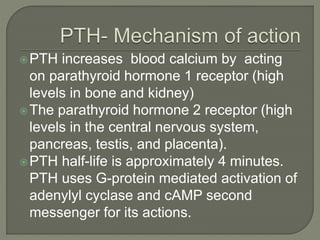
![ Secretion of parathyroid hormone is controlled
chiefly by serum [Ca2+] through negative
feedback.
Calcium-sensing receptors located on
parathyroid cells are activated when [Ca2+] is
low.
PTH is continuously produced and degraded.
When blood calcium is low, the degradation is
reduced and PTH is released.
When blood calcium is high, degradation is
increased and PTH is not released.](https://image.slidesharecdn.com/parathyroidhormone-200608111617/85/Parathyroid-hormone-8-320.jpg)
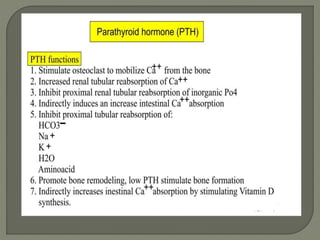
![ Secretion of parathyroid hormone is determined chiefly
by serum ionized calcium concentration thro negative
feedback.
Calcium binds calcium-sensing receptors on the cell
surface.
It results in activation of the Gq G-protein coupled
cascade through the action of phospholipase C
This hydrolyzes phosphatidylinositol 4,5-
bisphosphate (PIP2) to liberate intracellular
messengers IP3 and diacylglycerol(DAG).
It results in a release of calcium from intracellular stores
into the cytoplasmic space.
It inhibits release of PTH.
PTH is secreted when [Ca2+] is decreased](https://image.slidesharecdn.com/parathyroidhormone-200608111617/85/Parathyroid-hormone-9-320.jpg)