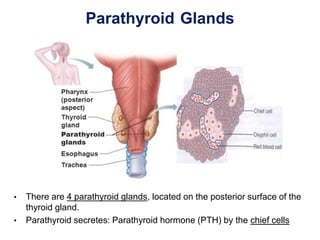
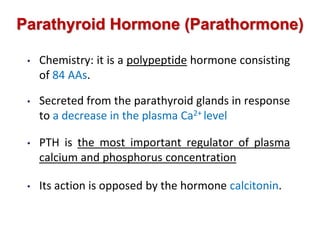
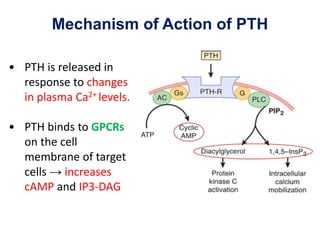
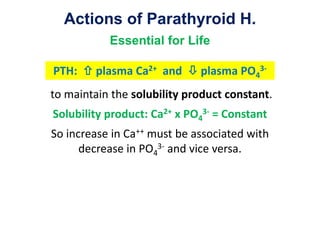
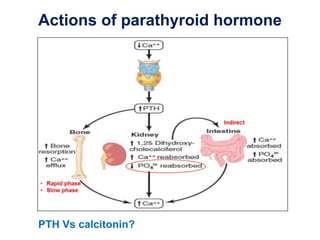
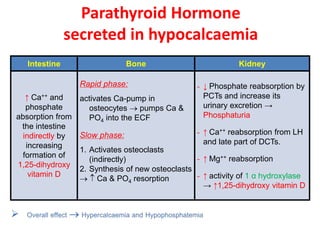
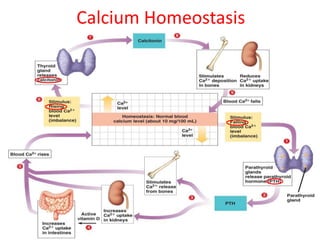
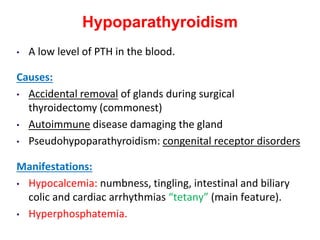
- There are 4 parathyroid glands located on the posterior surface of the thyroid gland that secrete parathyroid hormone (PTH), a polypeptide hormone. PTH increases calcium and decreases phosphate levels in the blood by acting on bone, kidney, and intestine. It mobilizes calcium from bone and increases calcium reabsorption in the kidney. PTH also increases vitamin D production, which further increases calcium absorption. Disorders of the parathyroid glands can lead to hypoparathyroidism or hyperparathyroidism and impact calcium and phosphate levels.
![Tetany
- Tetany is a state of increased neuromuscular excitability that
results from abnormally reduced plasma concentrations of
certain ions (Ca2+, Mg2+, or H+ [alkalosis]) → involuntary
spastic contraction of skeletal muscles.
- Manifest tetany: when plasma Ca2+ level is less 7 mg/dl
- Latent tetany: when plasma Ca2+ > 7mg % and < 9 mg%
- Pathophysiology: low Ca++ levels in ECF increase the
permeability of neuronal membranes to Na+ → progressive
depolarization](https://image.slidesharecdn.com/parathyroidhormone-200304083954/85/Parathyroid-hormone-17-320.jpg)