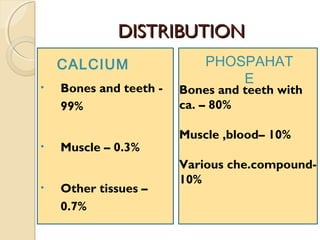
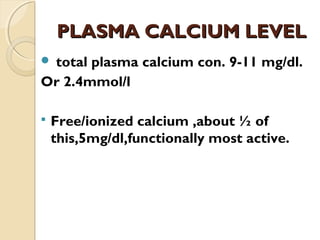
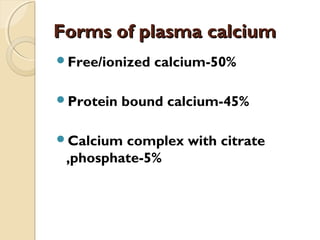
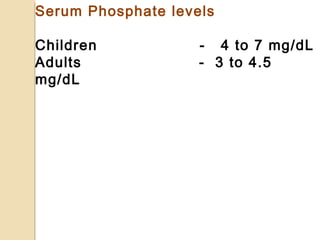
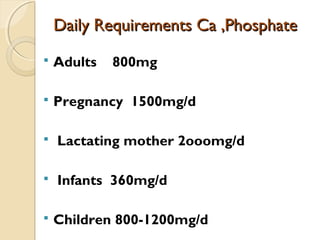
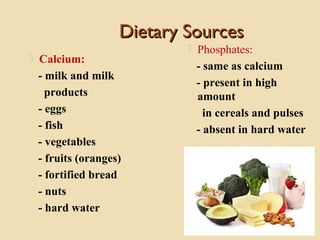
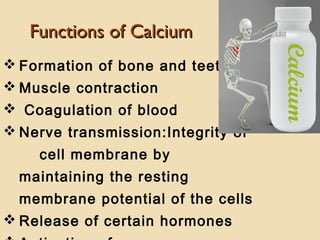
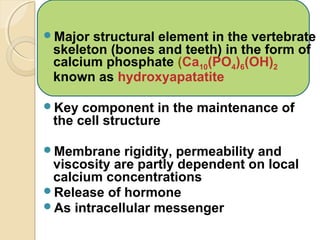
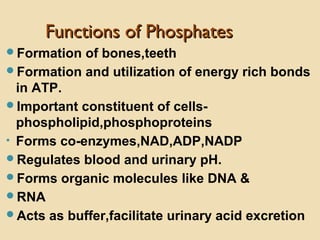
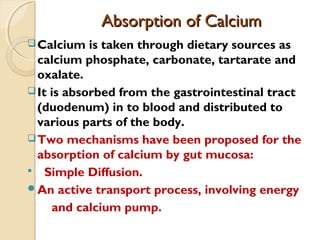
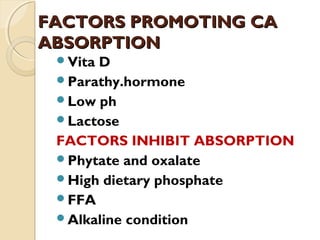
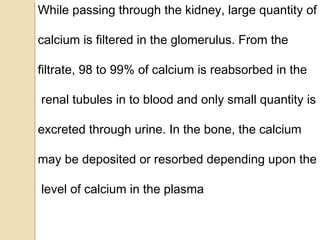
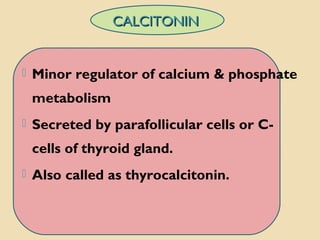
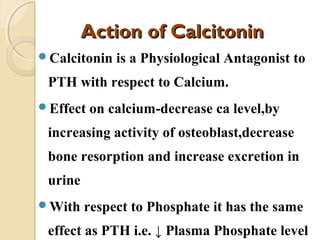
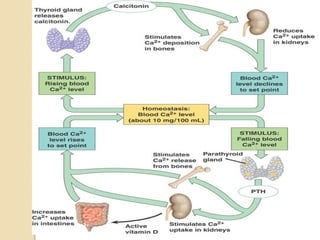
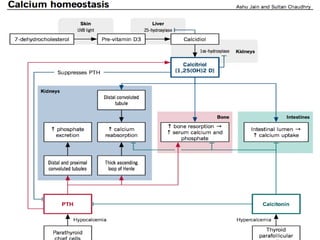
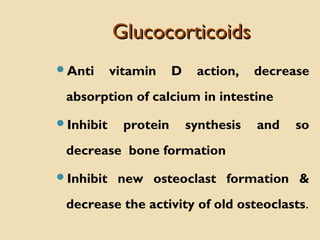
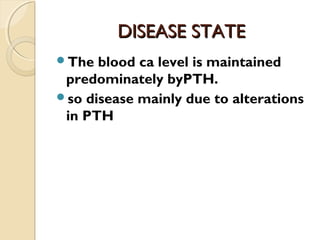
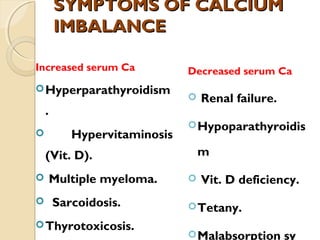
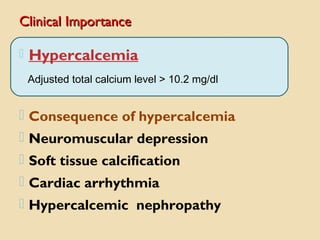
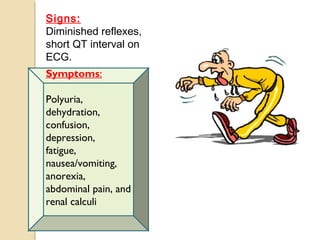
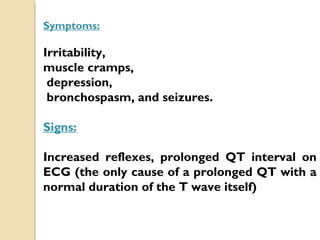
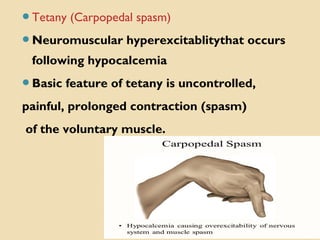
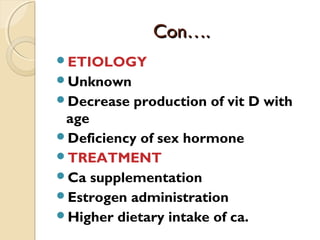
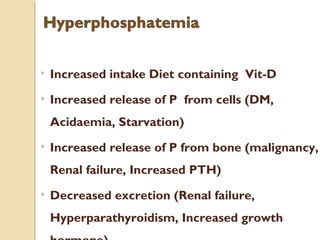
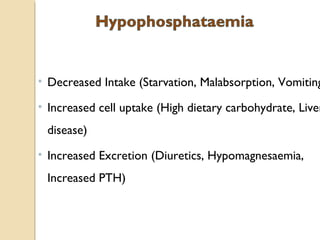
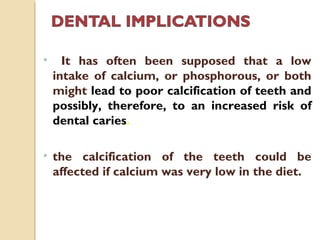
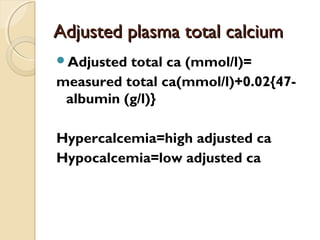
This document discusses calcium and phosphate metabolism and related disorders. It covers the distribution, functions, absorption and excretion of calcium and phosphate. It describes the roles of parathyroid hormone, vitamin D, and calcitonin in regulating calcium and phosphate levels. Disorders resulting from calcium and phosphate imbalance like hypercalcemia, hypocalcemia, rickets, and osteomalacia/osteoporosis are explained. Factors affecting calcium and phosphate levels and their clinical importance are also summarized.