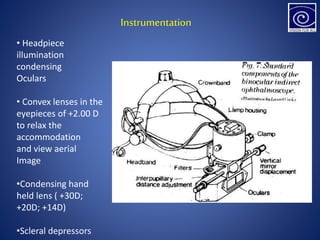
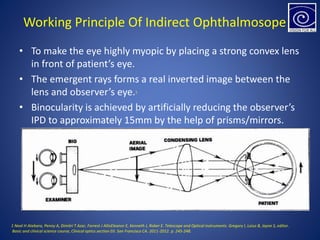
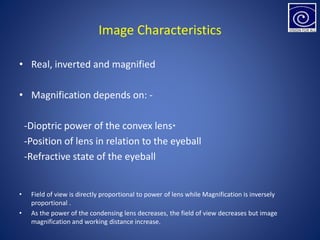
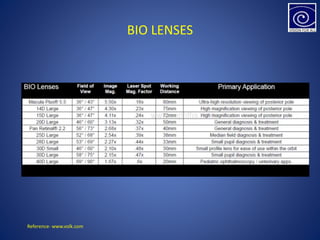
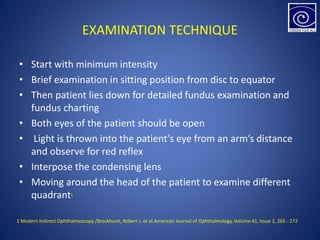
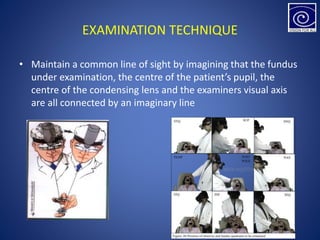
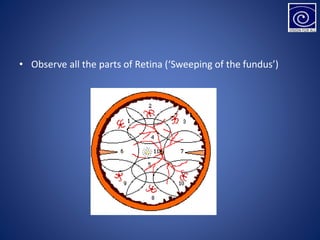
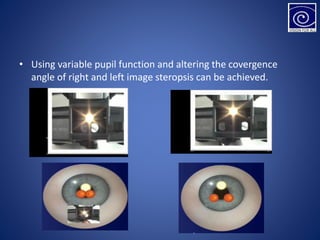
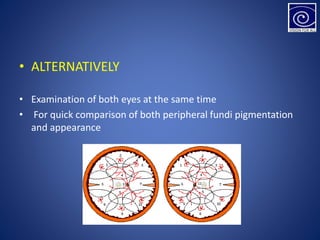
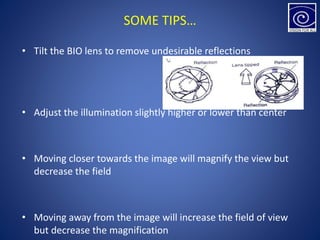
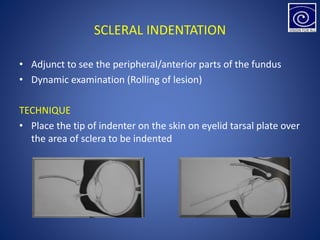
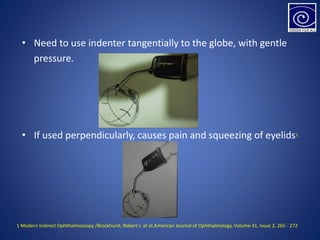
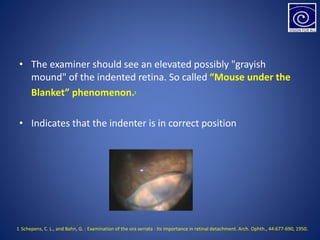
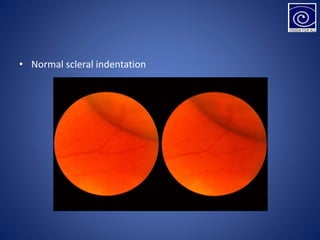
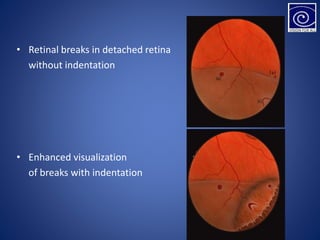
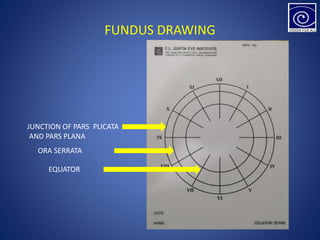
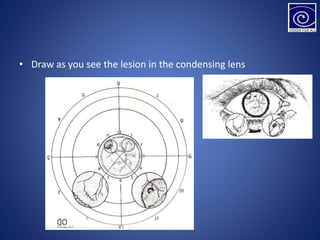
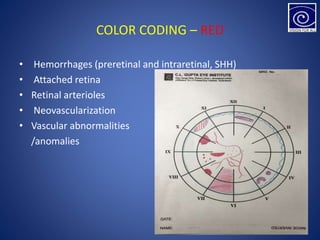
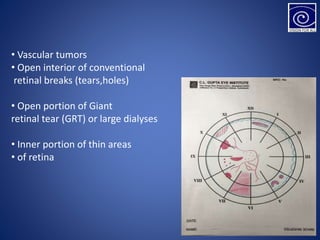
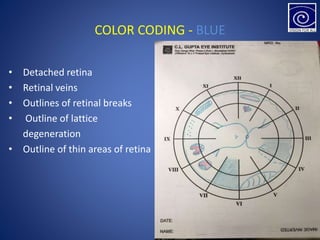
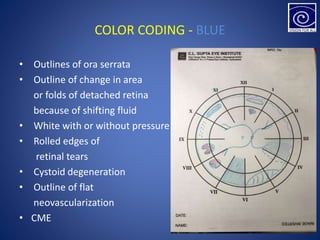
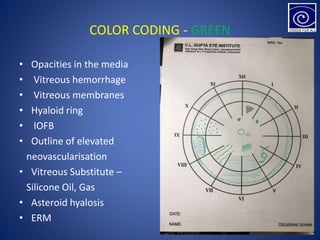
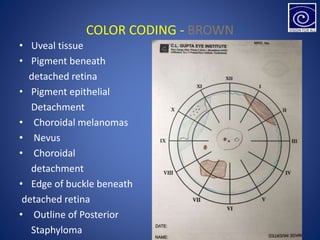
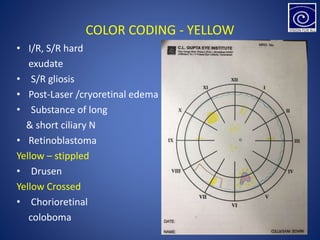
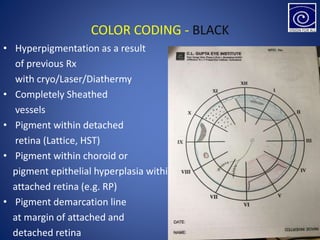
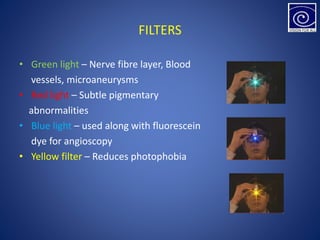
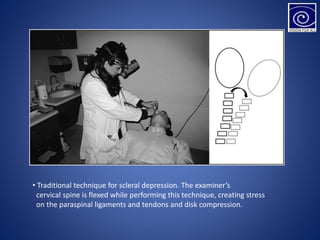
This document provides an overview of binocular indirect ophthalmoscopy and fundus drawing techniques. It discusses the history and working principles of the indirect ophthalmoscope. Examination techniques are described, including positioning, use of the condensing lens, and scleral indentation. Fundus drawing methods such as color coding retinal findings are also outlined. Proper cleaning and sterilization of equipment is emphasized.