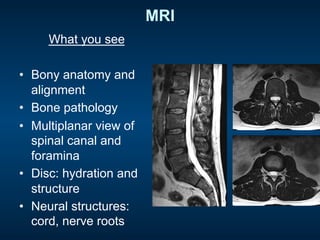
1) The document discusses appropriate imaging for back pain, describing different imaging modalities like X-rays, CT scans, bone scans, and MRI.
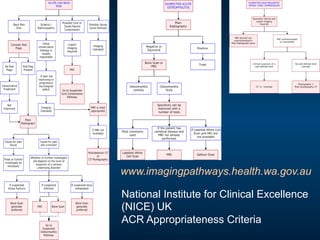
2) It categorizes back pain into 3 groups: nonspecific low back pain, back pain associated with radiculopathy, and back pain associated with a specific cause needing prompt evaluation.
3) Guidelines recommend triaging patients into these 3 categories and only imaging those with red flags, severe/progressive neurological symptoms, or if considering surgery/injections. Imaging is not recommended for nonspecific back pain.