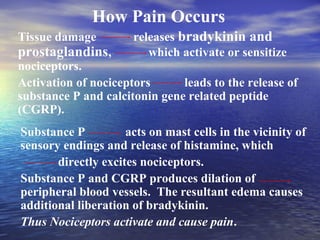
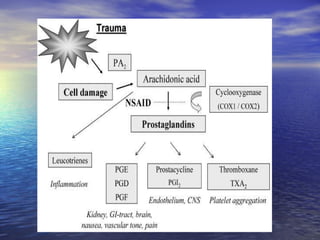
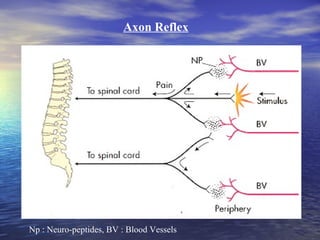
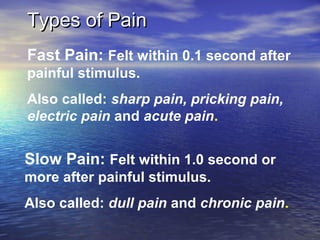
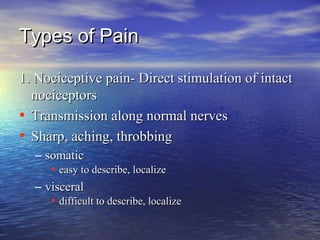
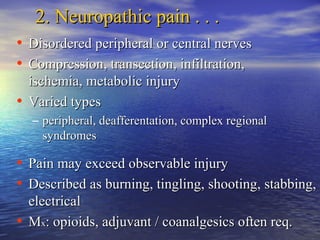
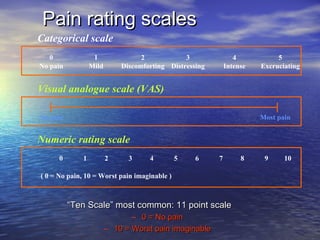
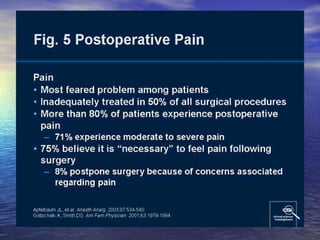
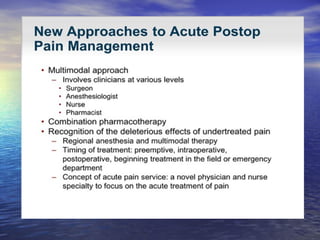
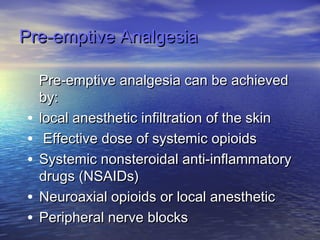
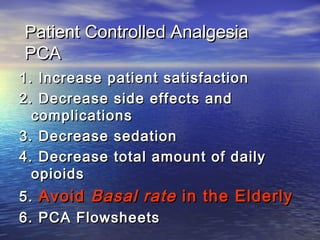
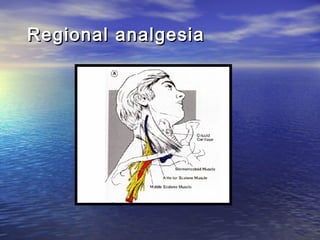
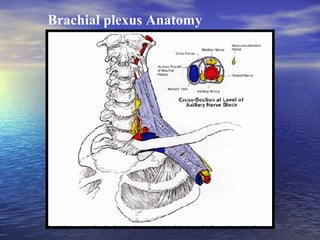
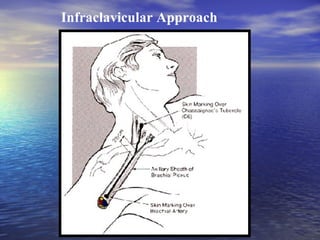
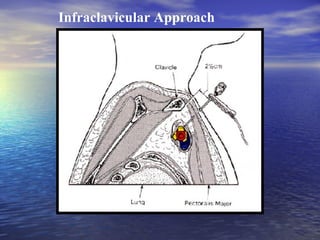
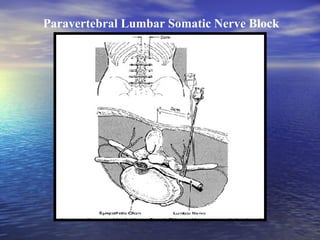
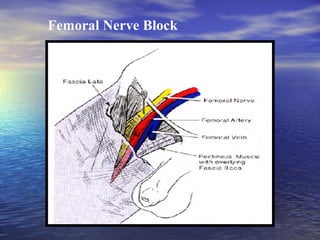
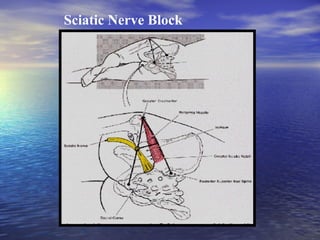
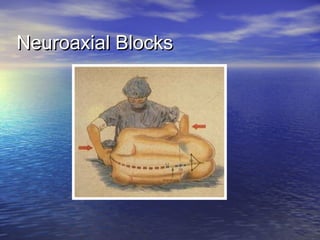
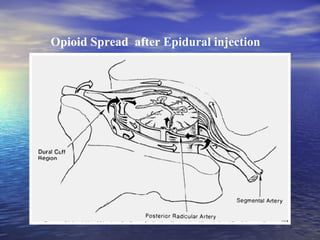
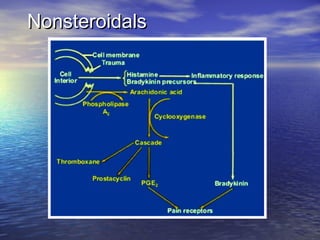
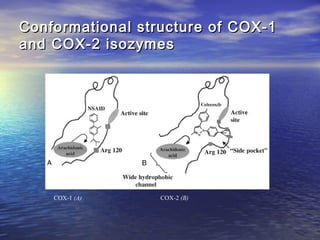
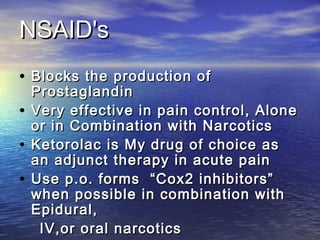
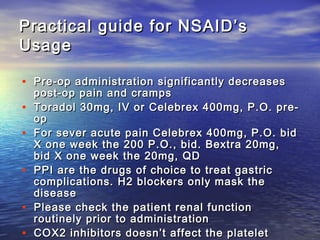
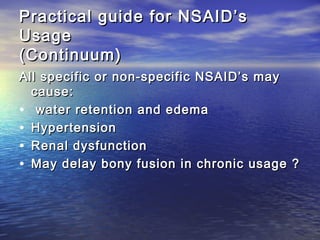
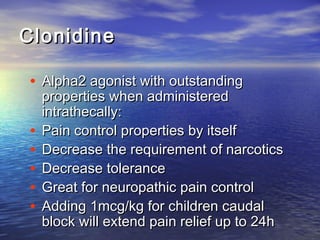
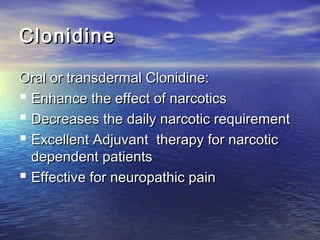
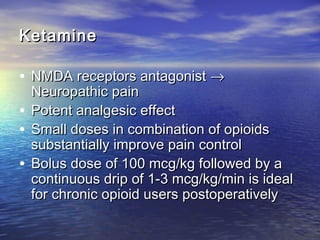
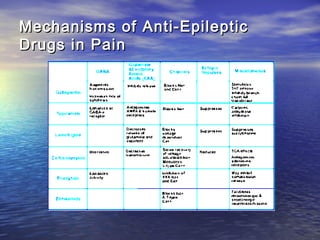
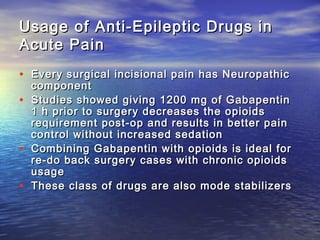
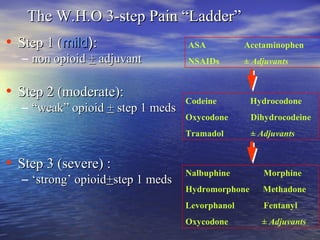
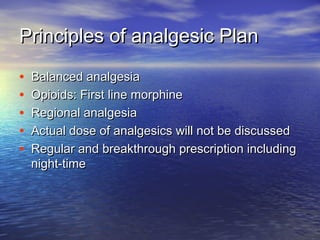
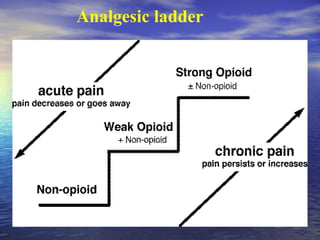
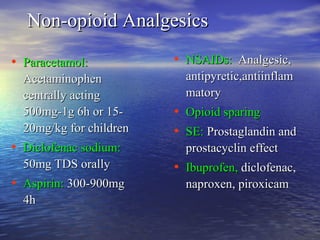
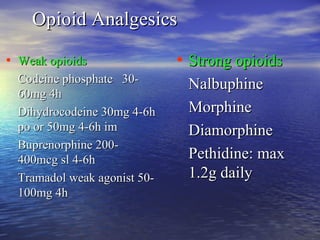
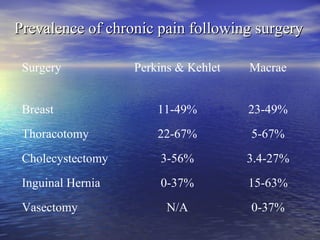
The document provides an overview of postoperative pain management, defining pain and discussing its pathways and mechanisms. It categorizes pain into nociceptive and neuropathic types, outlines pain assessment scales, and reviews various pain management modalities including opioid and non-opioid treatments, regional analgesia, and adjuvant therapies. It emphasizes a multidisciplinary approach and the importance of tailored analgesic plans for effective pain relief post-surgery.