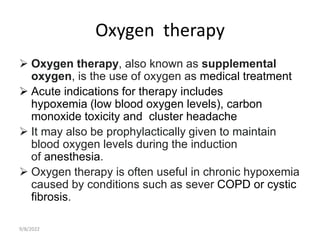
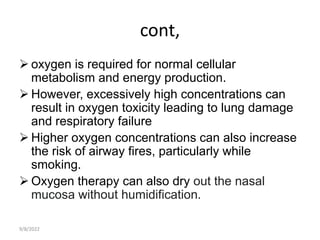
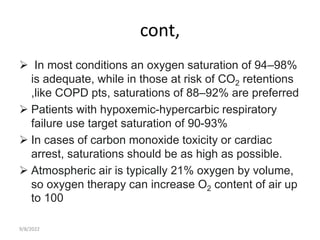
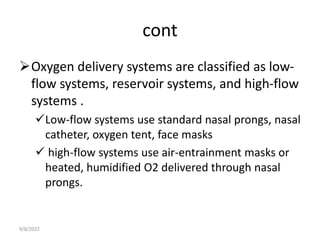
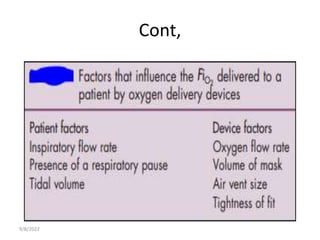
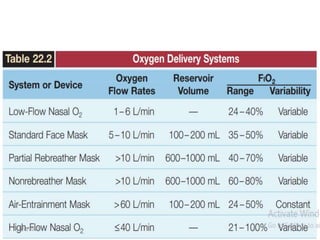
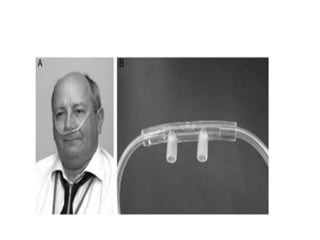
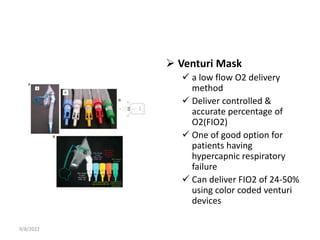
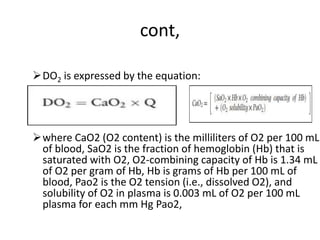
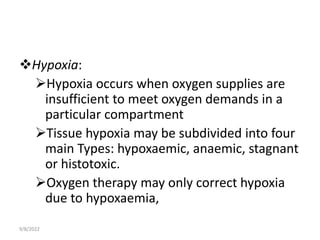
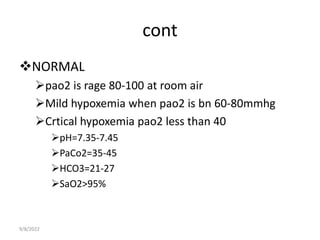
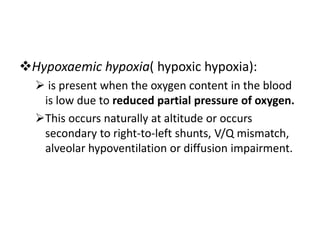
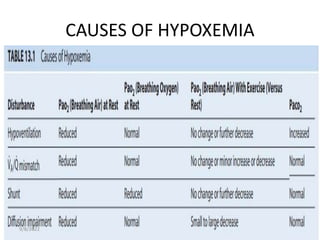
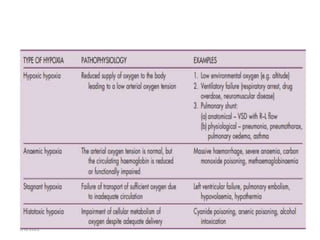
This document provides an outline and objectives for a lecture on oxygen therapy. It discusses normal oxygen levels in the body and how oxygen is transported. It describes different types of hypoxia and methods for oxygen delivery. Specific considerations are given for oxygen therapy in patients with obstructive lung diseases like COPD. Low-flow oxygen delivery systems like nasal cannulas and face masks are explained.
![cont,
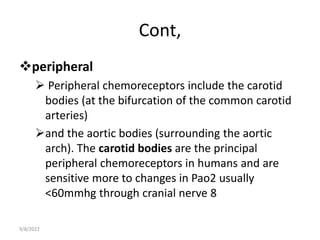
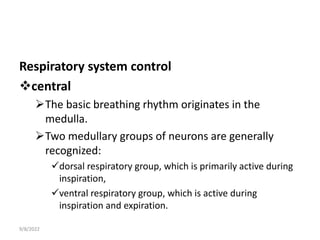
The most important of these sensors are
chemoreceptors that respond to changes in
hydrogen ion concentration
Central chemoreceptors are thought to lie on the
anterolateral surface of the medulla and respond
primarily to changes in cerebrospinal fluid [H+].
9/8/2022](https://image.slidesharecdn.com/oxygentherapy-220908204539-42bf41d9/85/oxygen-therapy-pptx-18-320.jpg)