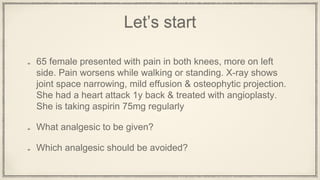
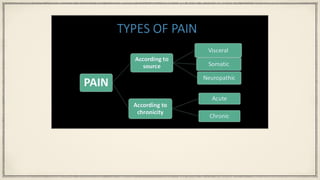
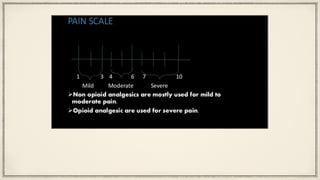
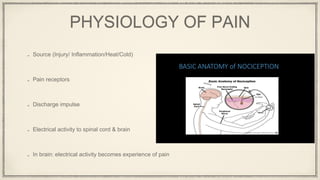
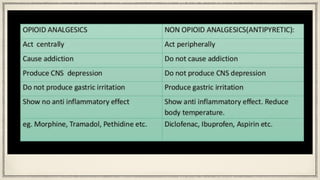
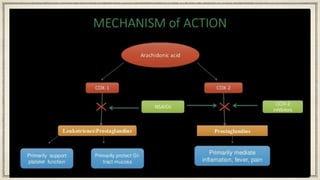
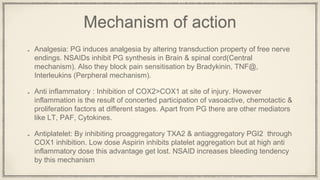
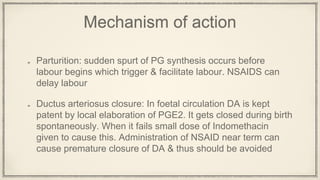
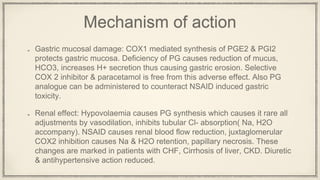
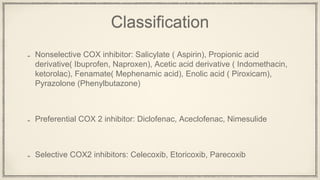
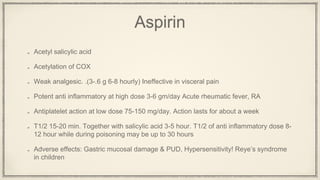
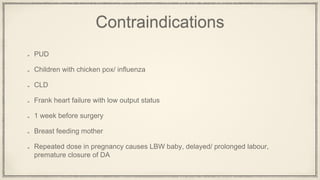
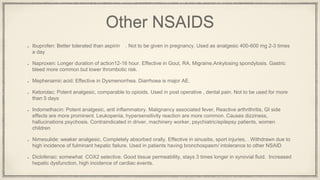
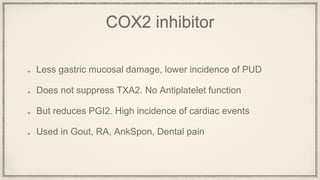
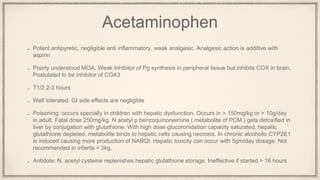
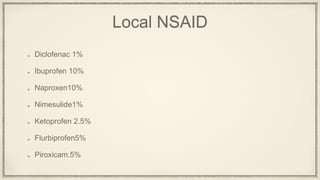
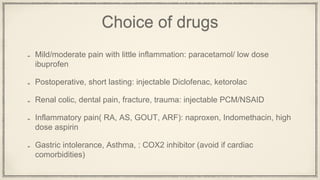
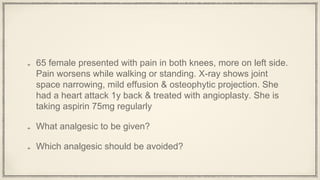
The document discusses the case of a 65-year-old female experiencing knee pain exacerbated by walking and standing, with imaging showing joint issues, and her history of a heart attack treated with angioplasty. It reviews the mechanisms, classifications, and effects of various analgesics, highlighting the use of NSAIDs, acetaminophen, and their contraindications, particularly for patients with specific health conditions. It emphasizes the importance of selecting appropriate analgesics based on safety and efficacy, especially in patients with a history of cardiovascular events.