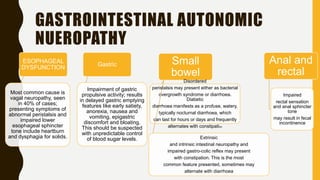
Diabetic patients have increased risk of complications during surgery due to microvascular and macrovascular changes caused by the disease. Autonomic neuropathy is common and affects the cardiovascular, gastrointestinal, genitourinary systems. It is important to assess for autonomic dysfunction preoperatively using tests like heart rate variability, gastric emptying tests, urodynamic studies to guide anesthesia management and reduce risks. Regional anesthesia is preferred over general anesthesia for patients with autonomic neuropathy due to the risk of hypotension, but careful titration is needed to avoid it. Strict glycemic control and protocols to reduce aspiration risk must also be followed in these high risk patients.