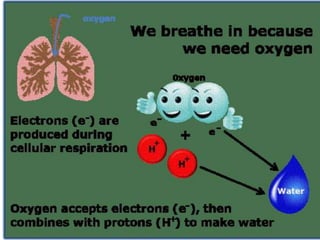
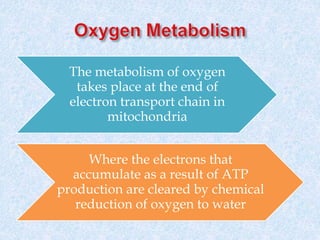
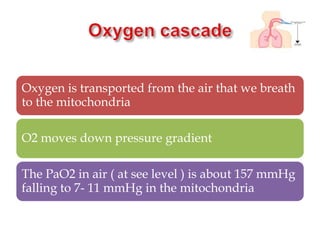
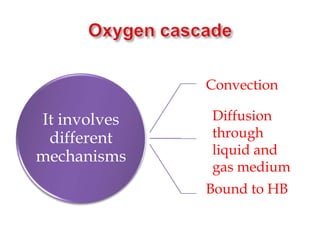
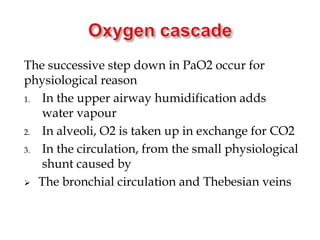
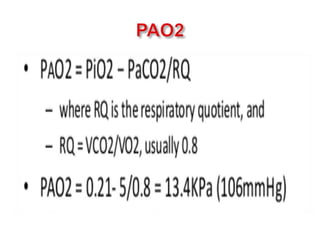
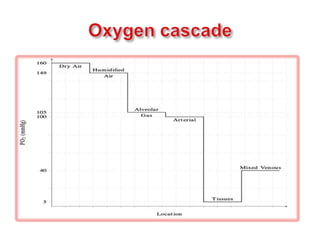
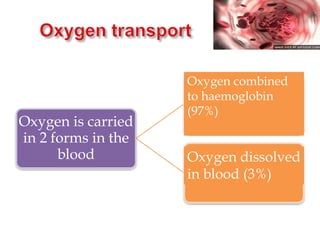
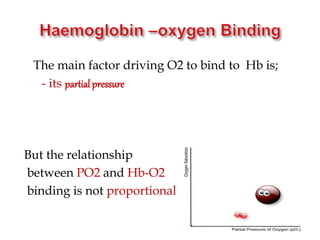
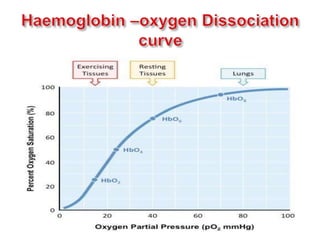
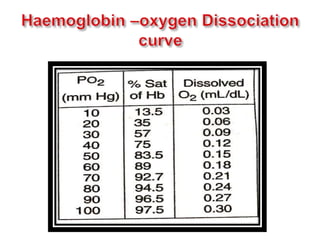
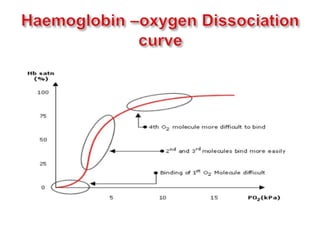
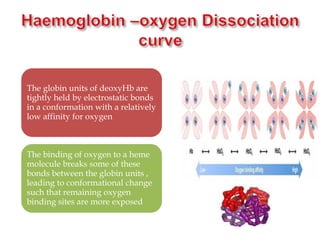
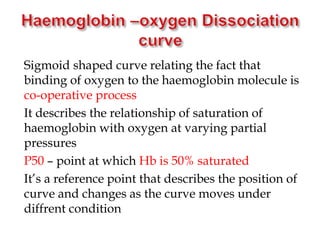
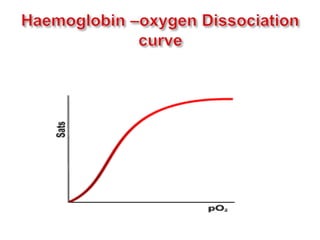
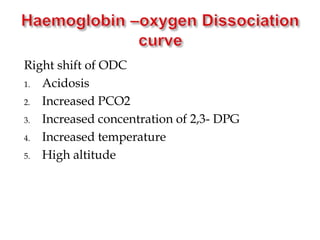
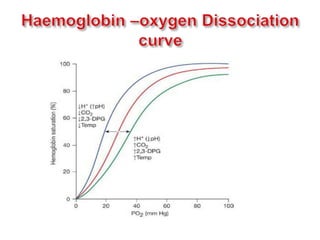
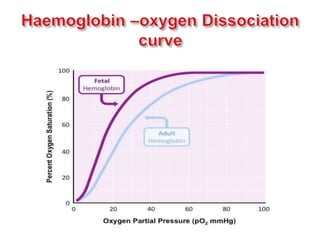
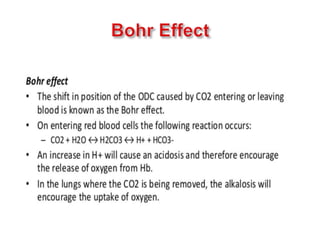
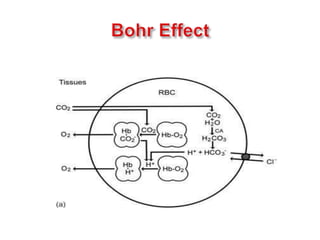
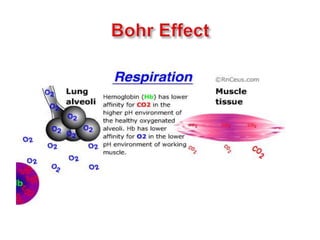
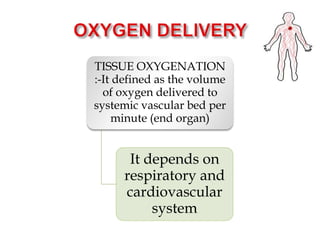
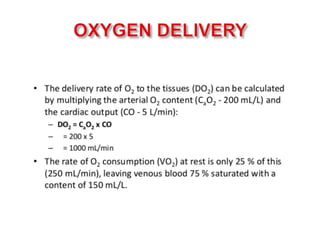
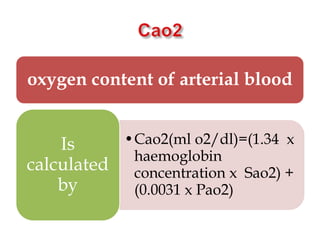
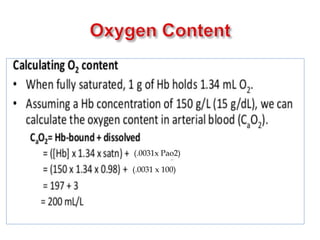
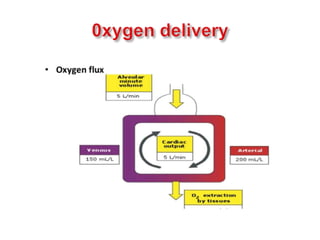
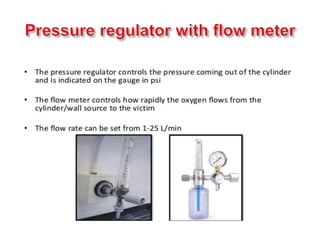
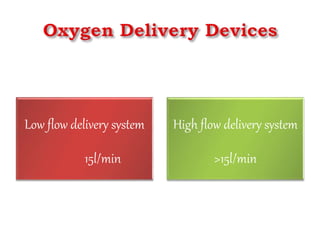
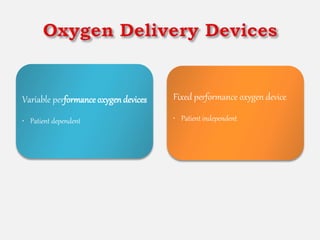
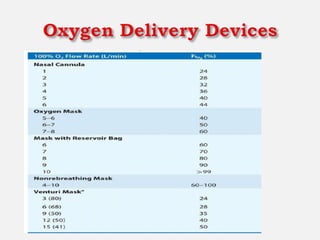
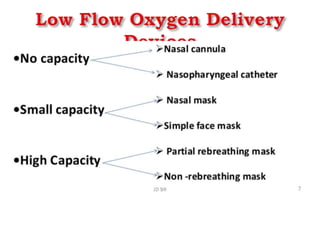
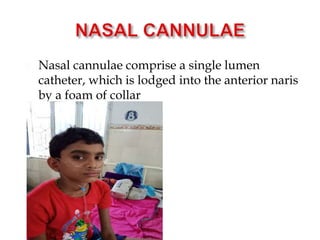
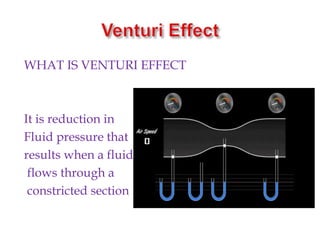
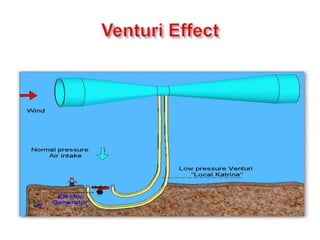
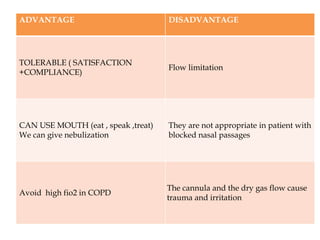
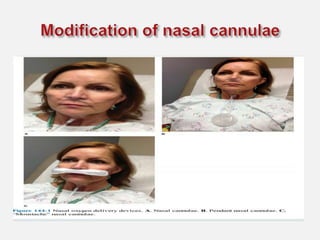
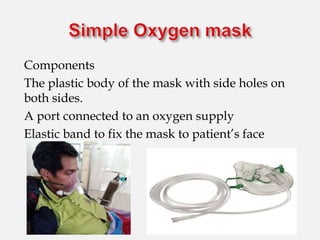
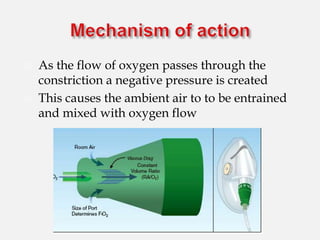
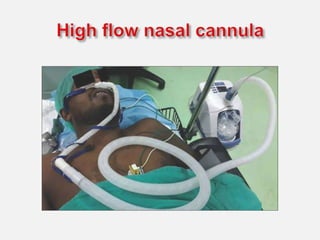
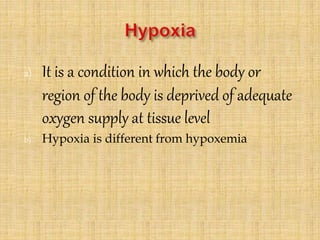
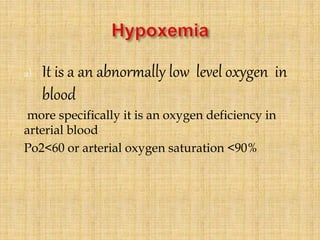
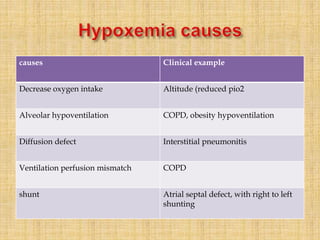
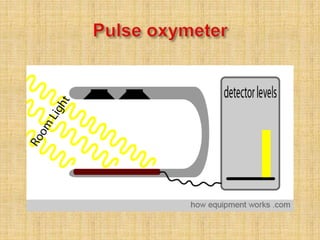
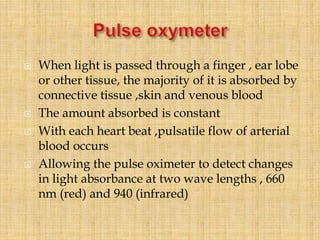
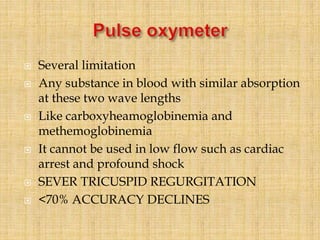
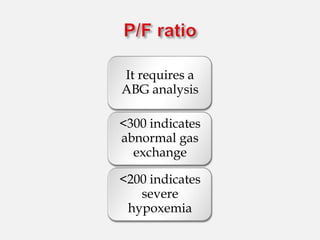
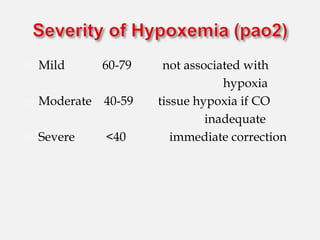
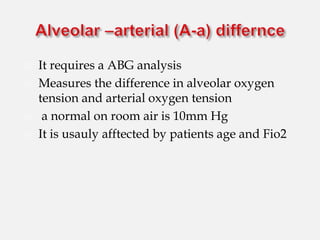
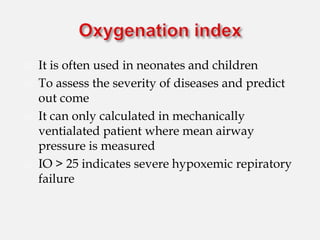
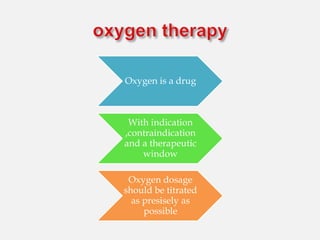
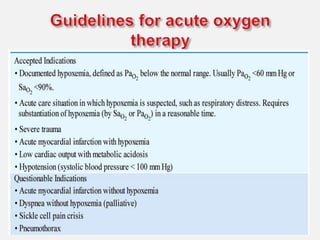
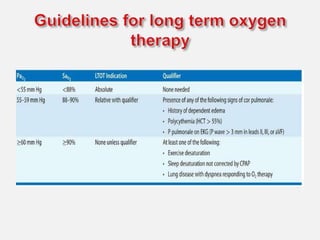
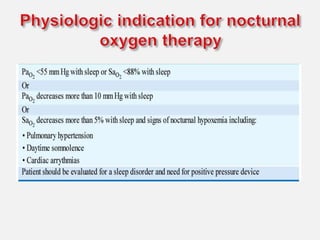
This document discusses oxygen properties, transport, and therapy. It describes how oxygen is transported from the lungs to tissues via hemoglobin in the blood. The oxygen-hemoglobin dissociation curve illustrates how various factors influence oxygen binding and release. Hypoxemia is defined as low oxygen levels in arterial blood, and can be caused by reduced intake, ventilation issues, or shunts. Pulse oximetry non-invasively measures arterial oxygen saturation to help guide oxygen therapy and identify hypoxemia. Various oxygen delivery devices are outlined that can precisely control inspired oxygen concentrations.