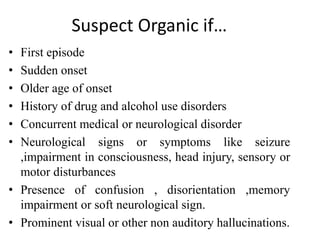
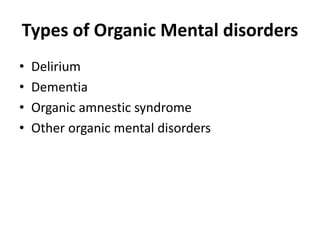
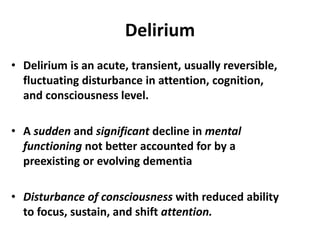
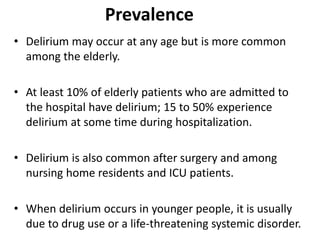
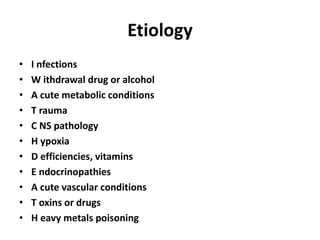
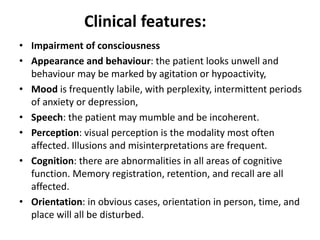
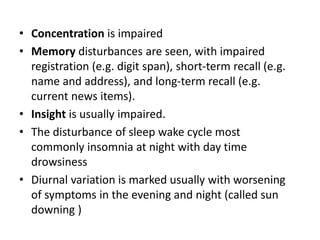
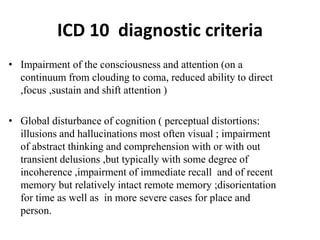
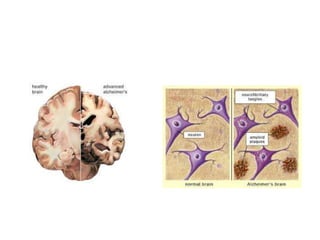
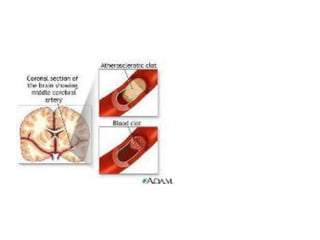
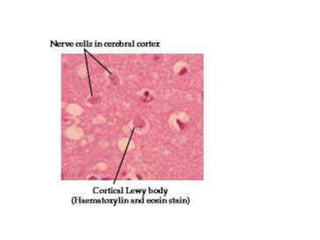
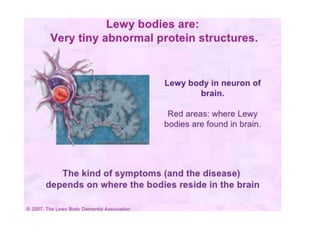
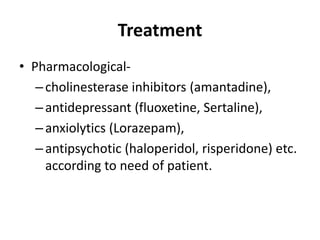
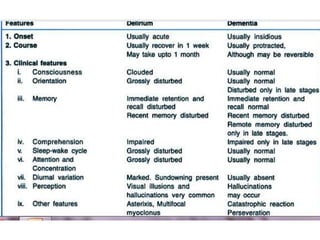
This document provides an overview of organic mental disorders, focusing on delirium and dementia. It defines delirium as an acute, transient disturbance in attention, cognition and consciousness that is usually reversible. Dementia is described as a chronic or persistent decline in cognitive abilities severe enough to interfere with daily life. The document outlines the prevalence, causes, signs/symptoms and diagnostic criteria for delirium. It also discusses the types and characteristics of dementia. Nonpharmacological and pharmacological treatment approaches are summarized for delirium, including addressing underlying causes and maintaining behavioral control.