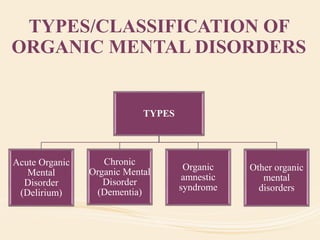
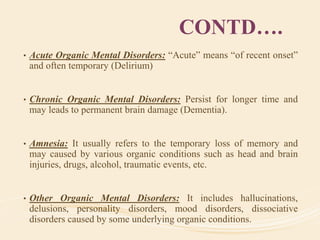
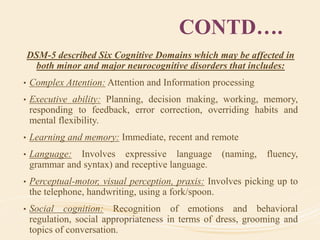
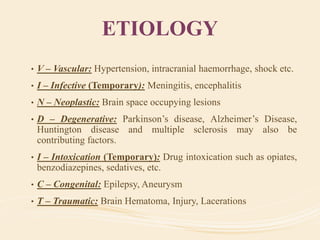
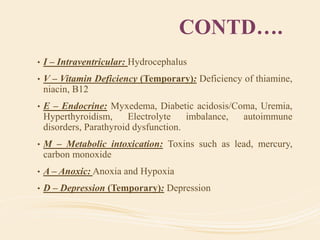
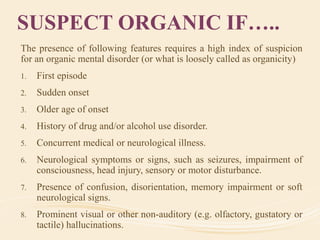
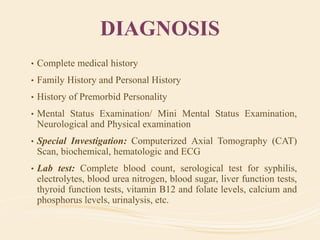
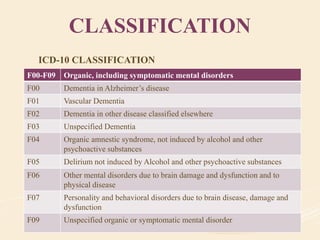
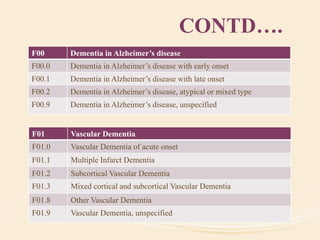
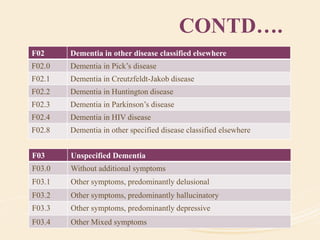
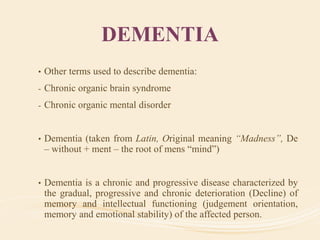
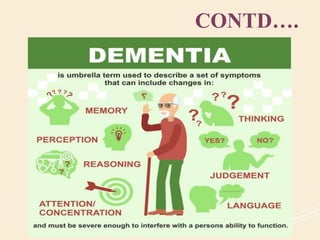
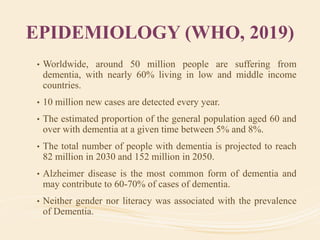
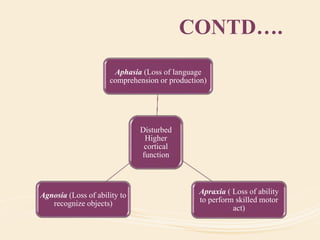
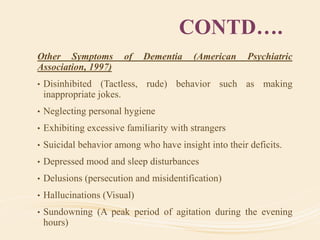
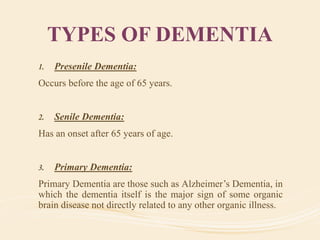
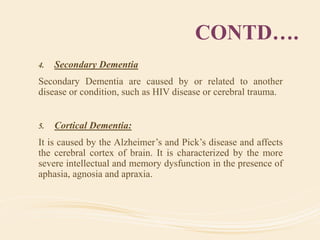
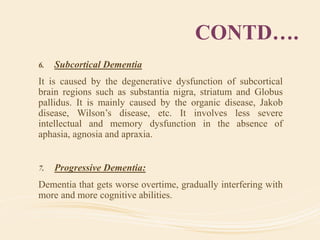
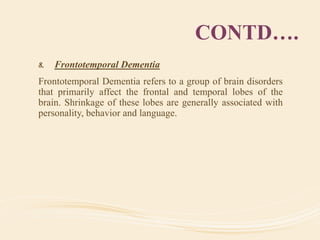
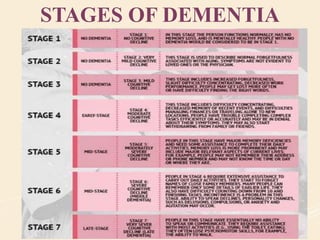
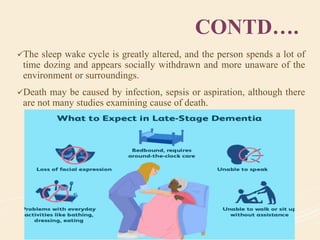
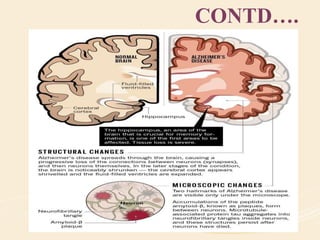
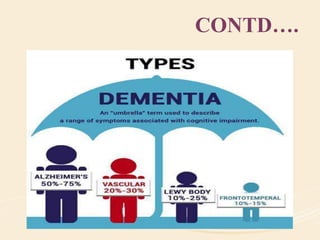
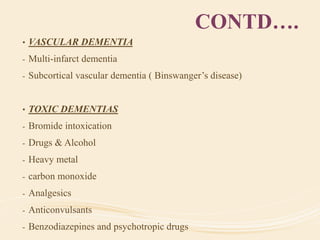
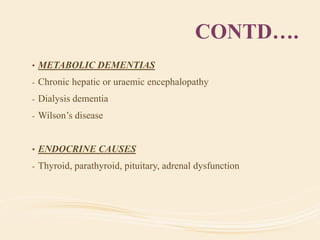
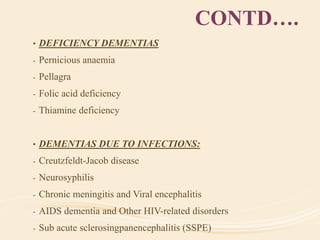
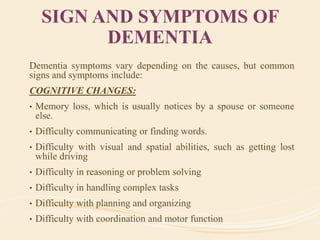
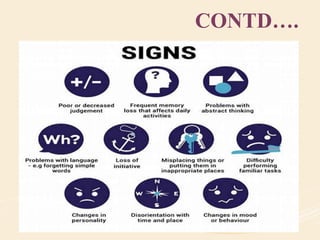
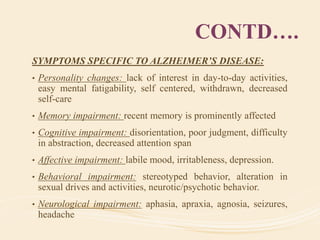
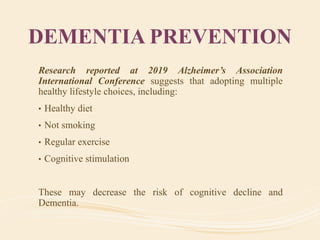
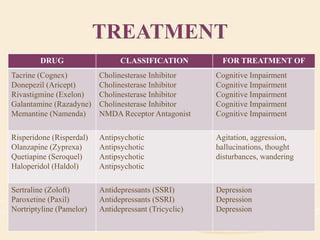
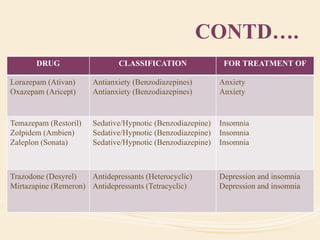
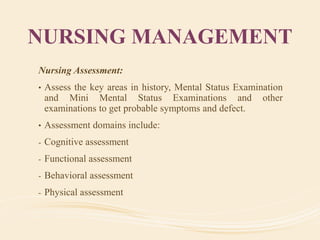
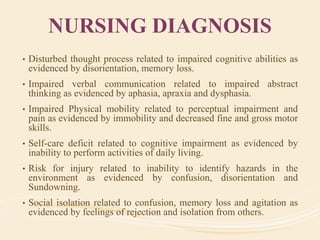
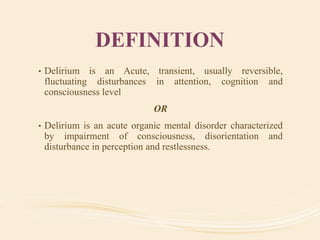
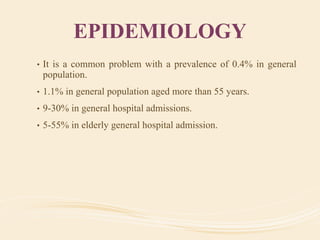
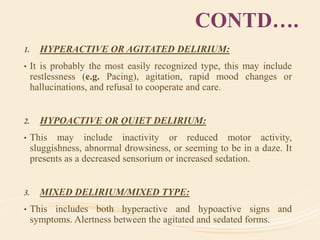
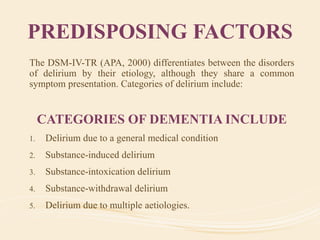
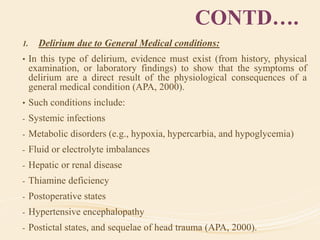
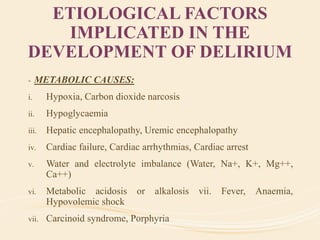
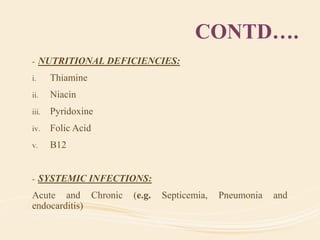
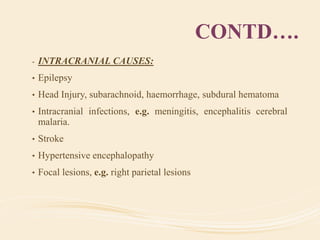
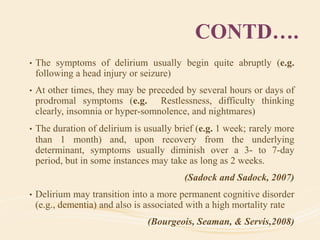
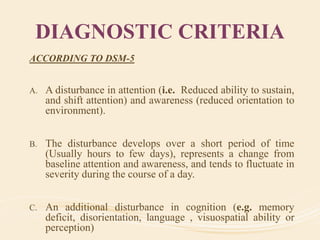
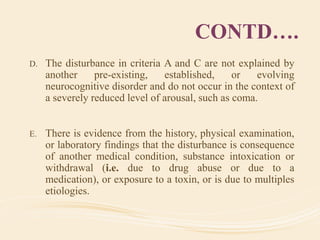
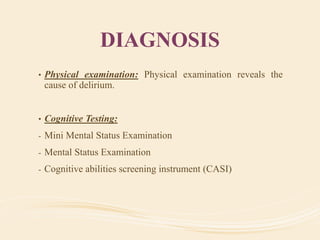
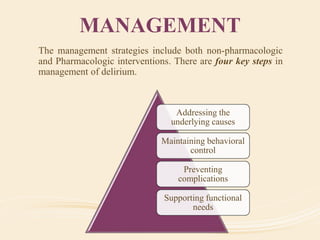
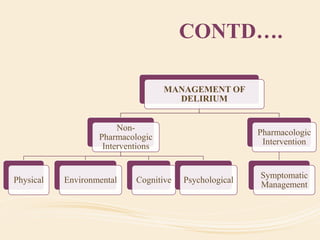
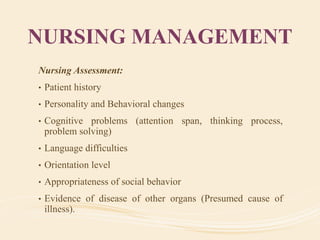
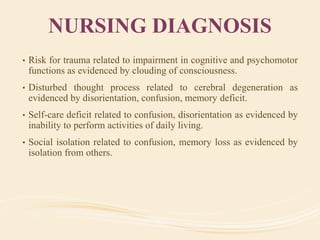
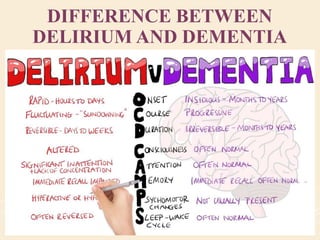
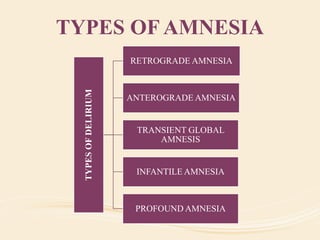
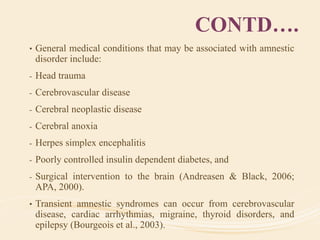
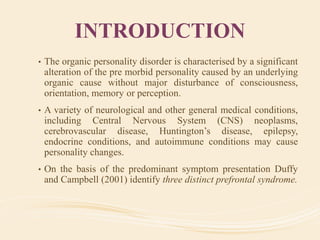
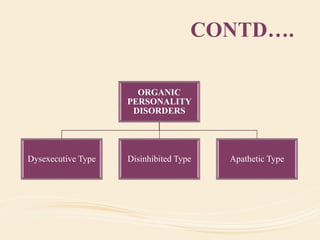
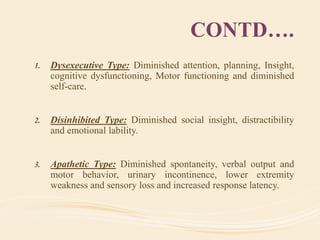
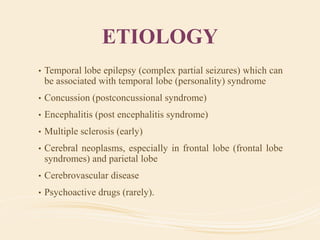
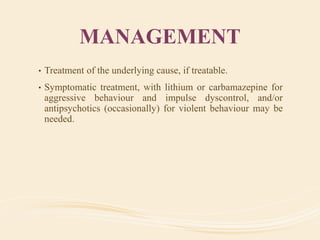
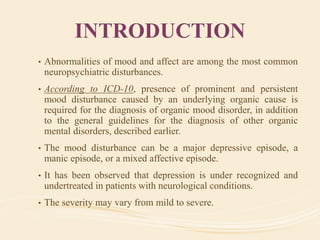
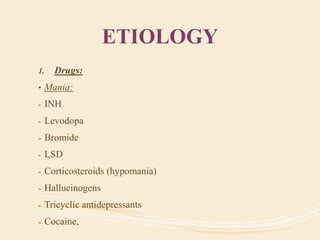
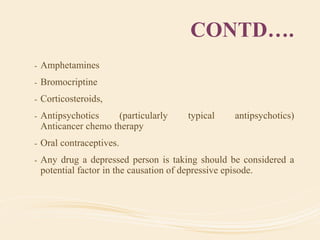
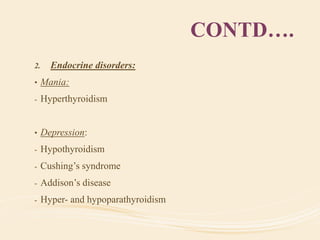
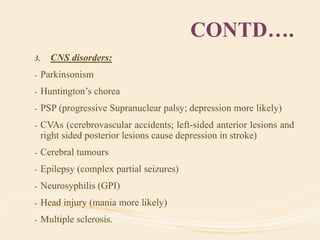
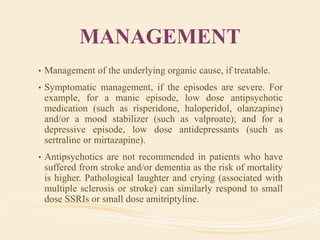
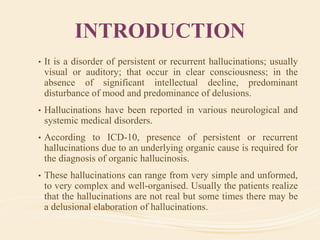
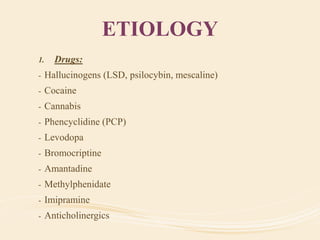
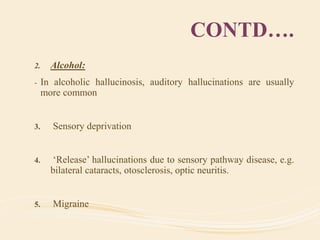
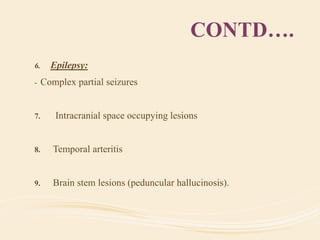
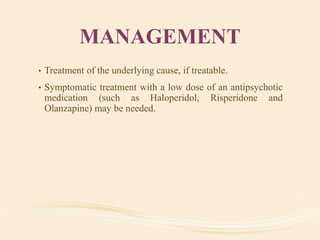
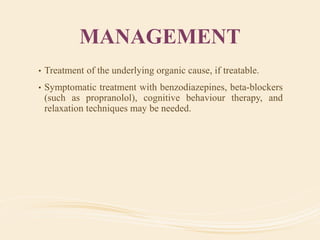
The document discusses organic mental disorders, particularly focusing on organic brain syndrome, cognitive deficits, and types such as acute and chronic organic mental disorders. It covers definitions, classifications, etiology, diagnosis, and the spectrum of dementia, illustrating its impact on cognitive and daily functioning. Furthermore, it highlights the prevalence of dementia and its stages, emphasizing the need for careful diagnosis and recognition of behavioral symptoms.