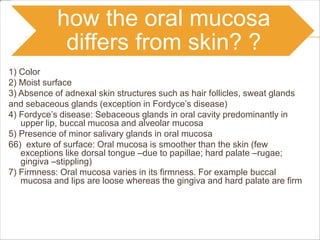
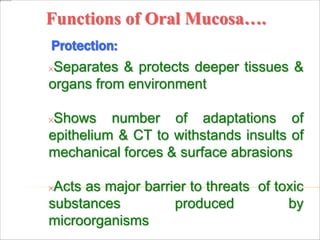
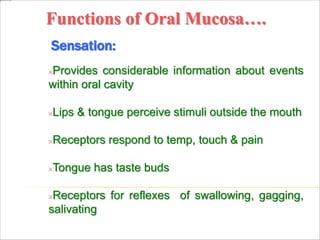
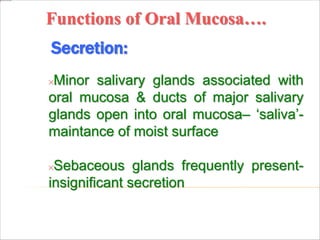
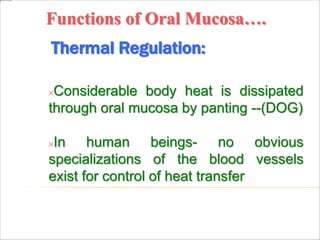
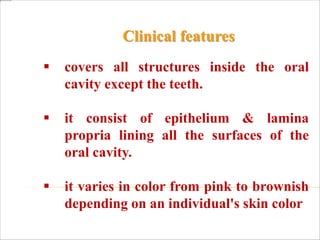
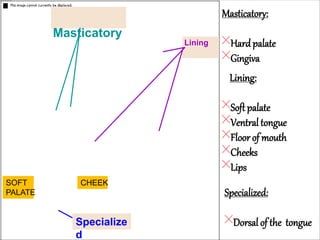
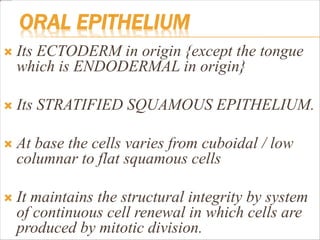
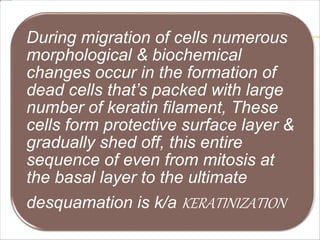
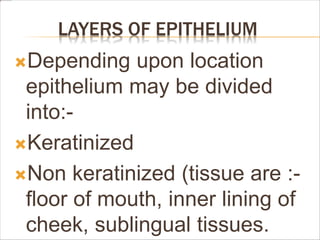
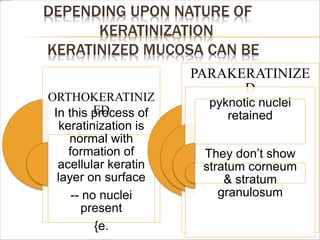
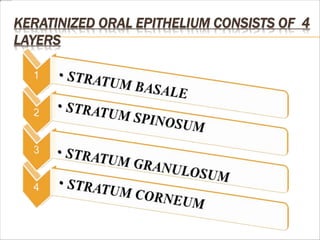
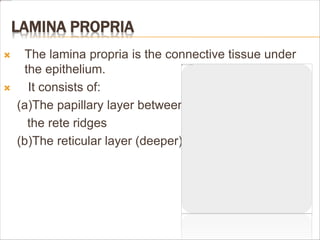
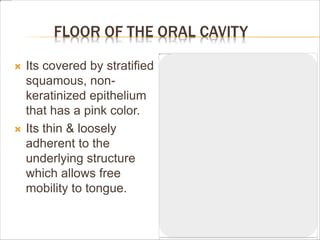
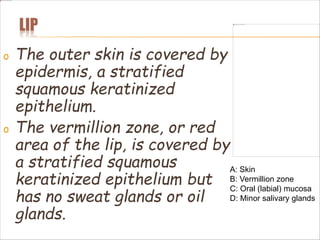
The oral mucosa is the moist lining of the oral cavity that continues with the skin and esophagus. It has three main functions - protection, sensation, and secretion. It protects the deeper tissues from mechanical forces and toxins, senses stimuli like temperature and pain, and secretes saliva through minor salivary glands. The oral mucosa varies between keratinized mucosa covering areas like the gingiva and hard palate, non-keratinized mucosa in areas like the floor of the mouth and cheeks, and specialized mucosa bearing taste buds on the tongue.
![Masticatory mucosa
It’s 25% of total mucosa.
It doesn’t stretch and is attached to bone.
During mastication it bears chewing forces.
It covers Gingiva [free{marginal}attached
and interdental] & hard palate.
Primary mucosa to be in contact with food
during mastication.
MASTICATORY MUCOSA IS USUALLY
KERATINIZED.](https://image.slidesharecdn.com/oralmucosa-210809034758/85/Oral-mucosa-18-320.jpg)

![PROTECTION
Oral Mucosa separates,& protects deeper
tissue /organs in oral regions from the
following:-
[a] Environment of oral cavity.
[b] Mechanical forces of biting & mastication ,to
surface abrasion from hard particle in diet.
[c] Microorganisms may cause infection if they get
access into the underlying tissue.
[d] Toxins produced by micro organisms.](https://image.slidesharecdn.com/oralmucosa-210809034758/85/Oral-mucosa-43-320.jpg)
![HISTOLOGY OF ORAL MUCOSA
These layer separated by:-
(a)BASAL LAMINA [originate by
epithelium]
(b)BASEMENT MEMBRANE
[originate by connective tissue]
The connective tissue projection into
epithelium called PAPILLA.
The epithelium projection into lamina
propria are called EPITHELIAL](https://image.slidesharecdn.com/oralmucosa-210809034758/85/Oral-mucosa-50-320.jpg)
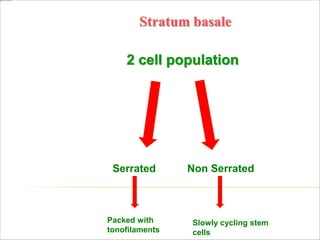
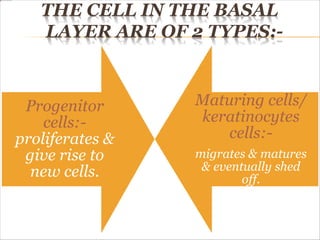
![THERE ARE 2 TYPES OF BASAL CELLS
• Packed with
tonofilaments
SERRATED
• made up of slowly
cycling stem cells [give
rise to amplifying cell
for cell division]](https://image.slidesharecdn.com/oralmucosa-210809034758/85/Oral-mucosa-64-320.jpg)
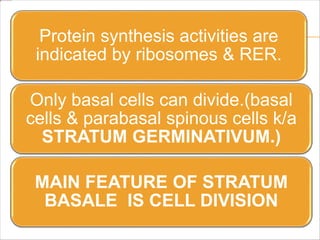
![ Serrated basal cells are single layer cuboid
cells ,these are packed with tonofilaments.
Have protoplasmic process which projects from
basal surface towards connective tissue, where
hemidesmosomes are present.
Adjacent cells consist of adjacent cell
membrane & pair of denser region & are
attached by desmosomes
Cell junction may be present [tight ,close & gap]](https://image.slidesharecdn.com/oralmucosa-210809034758/85/Oral-mucosa-65-320.jpg)
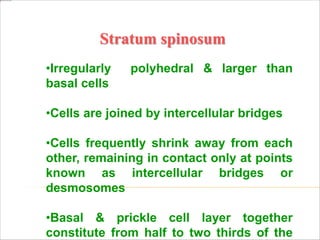
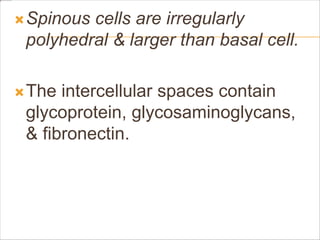
![STRATUM SPINOSUM
Also k/a prickle cell layer
[ because of cell shape]
When cells of this layer
shrinks away ,remaining in
contact only at 1 point k/a
INTERCELLULAR BRIDGE/
DESMOSOMES which gives
cells a spiny like profile.](https://image.slidesharecdn.com/oralmucosa-210809034758/85/Oral-mucosa-68-320.jpg)
![STRATUM GRANULOSUM
Cells are flat & wide [3-5 cells thick] larger
than spinous layer.
Prominent in keratinized epithelium &
deficient in non keratinized epithelium.
Having numerous dense , small
KERATOHYLINE GRANULES (granules in
the stratum granulosum ,which helps in
production of dead layer of cells on skin
surface), stains intensely with basic dye.](https://image.slidesharecdn.com/oralmucosa-210809034758/85/Oral-mucosa-72-320.jpg)
![ Under light microscope,
granules are basophilic
[blue with hematoxylin
stain] & under electron
microscope they are
dense [appearing
black]](https://image.slidesharecdn.com/oralmucosa-210809034758/85/Oral-mucosa-73-320.jpg)
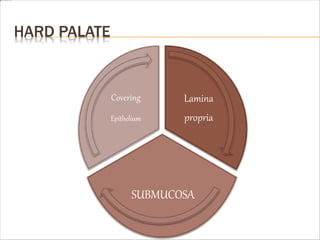
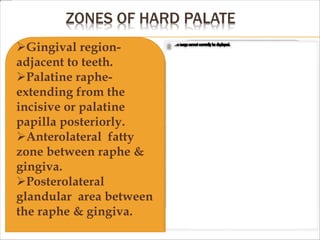
![COVERING EPITHELIUM
Epithelium of hard palate is thick
orthokeratinzed.
[some parts may show
parakeratinization],stratified
squamous epithelium &
anterolaterally its transverse
palatine ridges {rugue}.](https://image.slidesharecdn.com/oralmucosa-210809034758/85/Oral-mucosa-87-320.jpg)



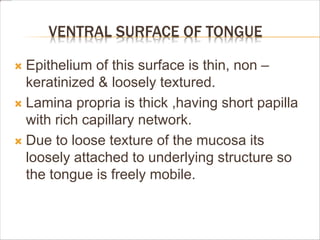
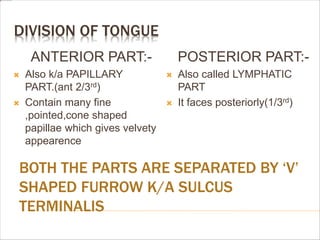
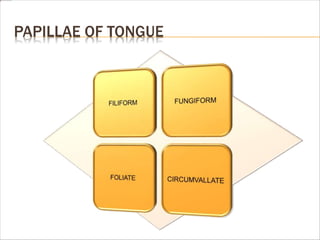
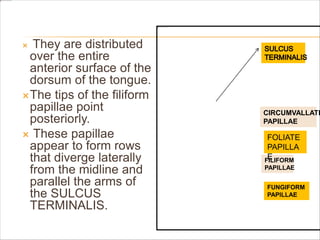
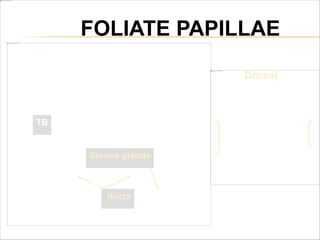
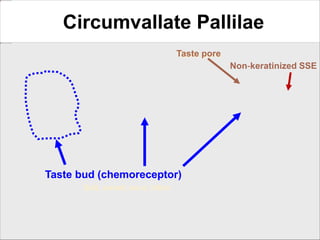
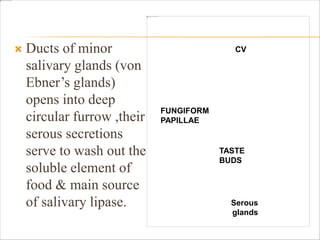
![SPECIALIZED MUCOSA [TONGUE]
Dorsal surface of tongue is covered by
specialized mucosa.
It’s non keratinized.
Containing numerous papilla having taste buds.
Anterior 2/3rd supplied by TRIGEMINAL NERVE
through its lingual branch.
Posterior 1/3rd supplied by
GLOSSOPHARYNGEAL NERVE.](https://image.slidesharecdn.com/oralmucosa-210809034758/85/Oral-mucosa-132-320.jpg)