The document provides a detailed overview of the oral mucosa, describing its definition, functions, and structural classification. It explains the components of the oral mucosa, including the epithelial layers, connective tissue, and the various types of junctions between cells. Additionally, the document discusses the anatomical and functional characteristics of the oral epithelium, including keratinization processes and the roles of different cell types and structures within the mucosa.
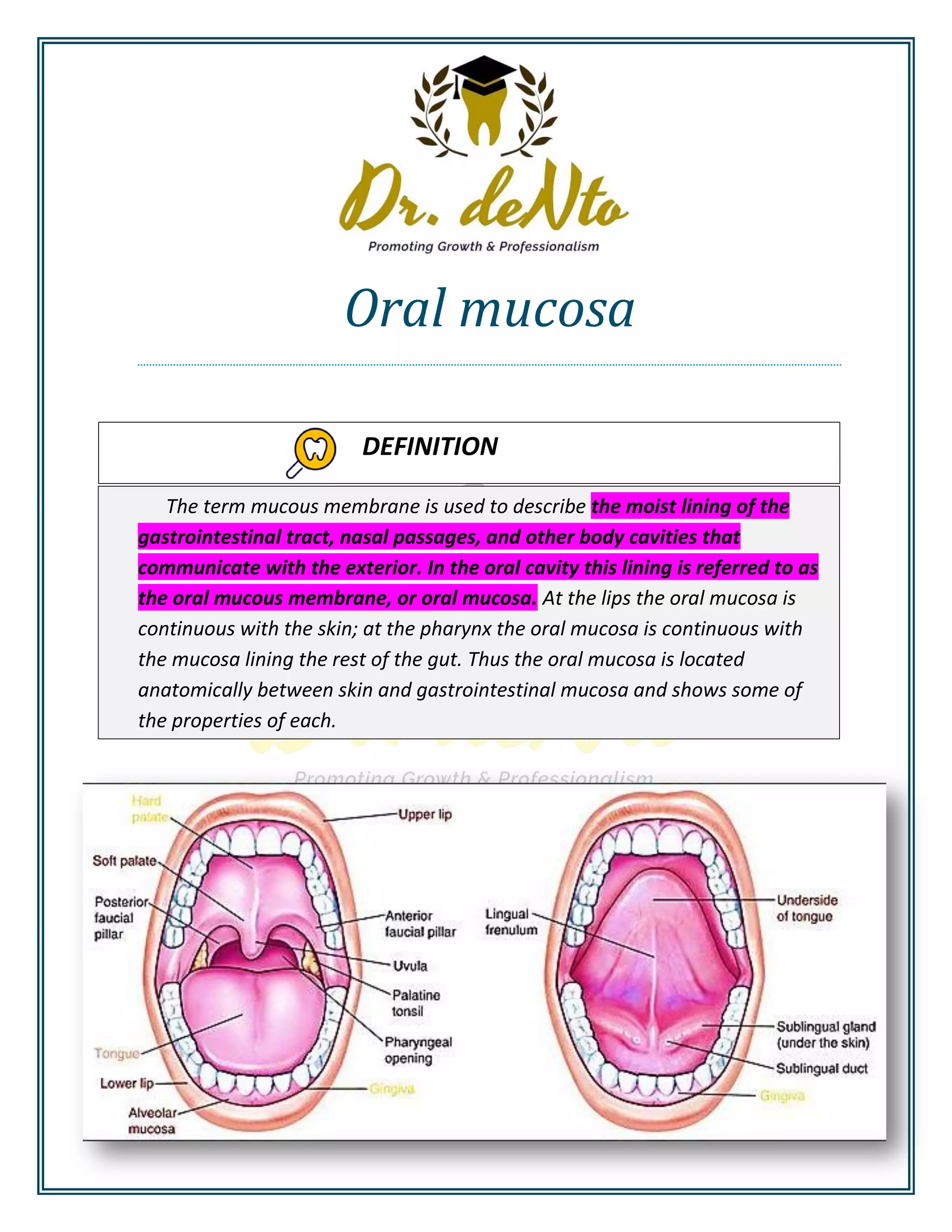


























![KERATINOCYTES 90% NON-KERATINOCYTES 10%
Cells have tonofilaments
That synthesize Cytokeratin(type
of intermediate filaments)
Desmosomes
Show cell division, maturation
and desquamation.
Don’t turn into keratinocytes or
share in keratin formation
Have a clear halo around the
nucleus, and so known, clear
cells.
Lack desmosomes except Merkel
cells.
Not stained with routine H&E
stain.
Not arranged in layers but found
scattered in mucosa.
Don’t show cell division,
maturation and desquamation.
NON-KERATINOCYTES
Depending of the position , the clear cells are divided into
1. Low - level clear cells ( melanocytes and merkel cells ) [ basal ]
2. High level clear cells ( langerhans cells )( supra - basal )](https://image.slidesharecdn.com/oralmucosapdf-200917162953/75/Oral-mucosa-membrane-28-2048.jpg)



