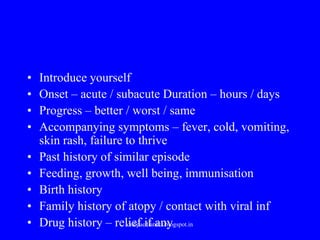
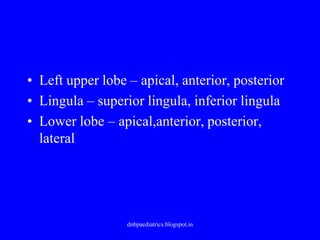
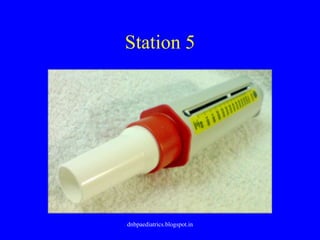
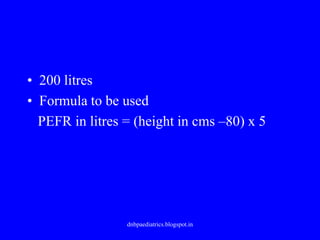
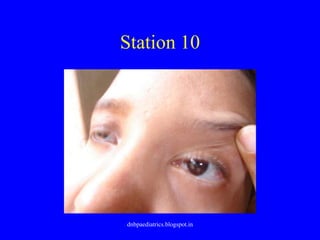
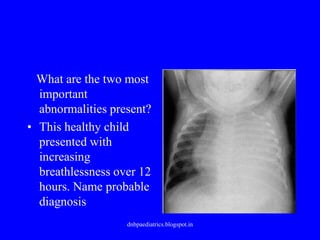
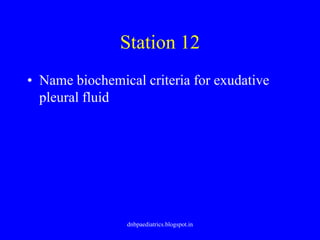
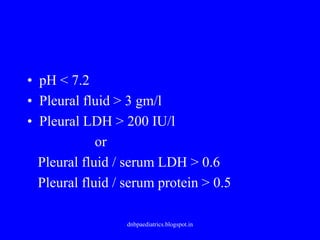
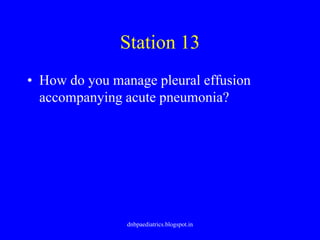
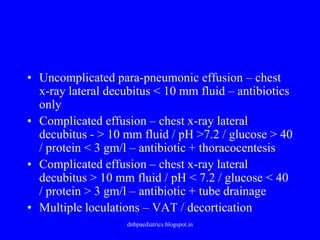
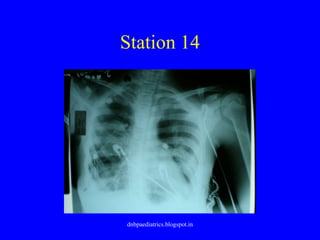
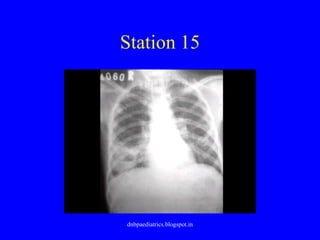
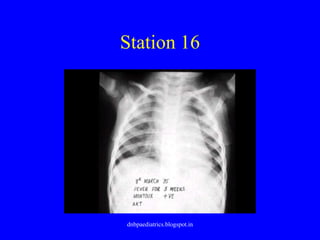
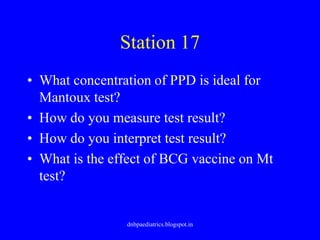
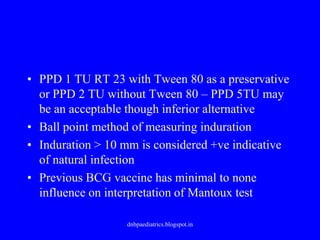
This document summarizes the stations and tasks involved in an OSCE (Objective Structured Clinical Examination) in pediatrics. It describes the history taking, physical exam, counseling, and diagnostic skills that would be evaluated at each station, including assessing a child with cough and wheezing, examining respiratory system, counseling parents of a child with asthma, evaluating lung anatomy and function, interpreting tests, and diagnosing and managing various respiratory conditions.