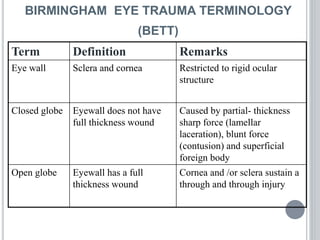
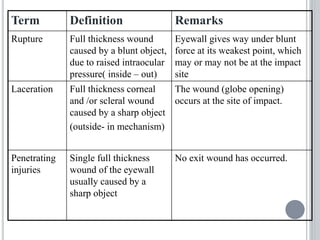
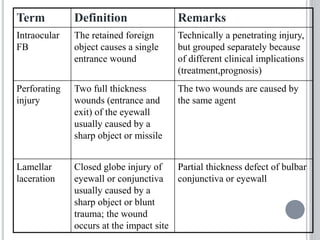
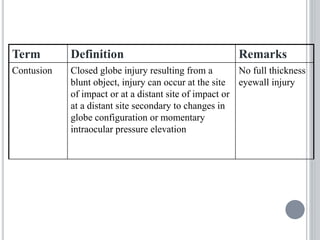
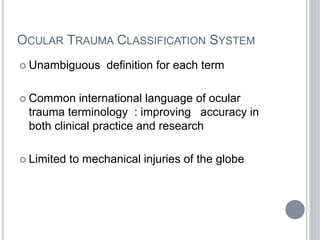
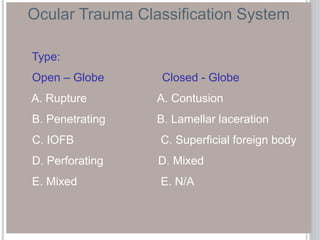
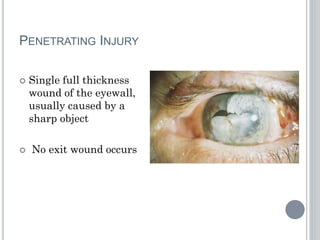
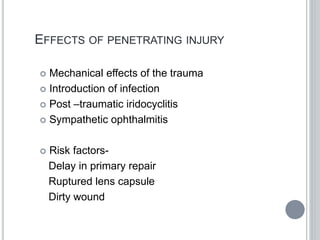
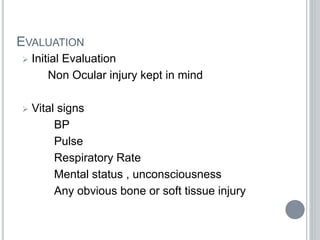
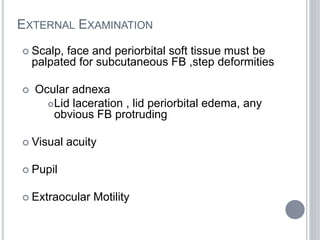
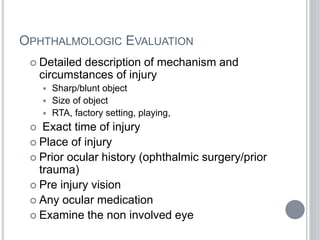
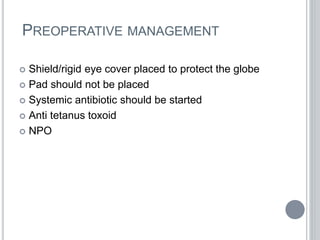
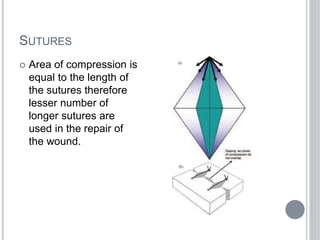
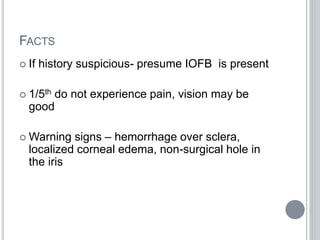
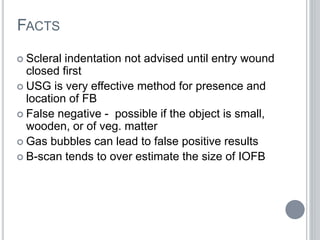
Penetrating ocular trauma can cause blindness and is commonly caused by sharp objects in men aged 15-34 years. A full thickness wound where the eyewall is penetrated is called an open globe injury, while an injury without a full thickness wound is a closed globe injury. Surgical repair of open globe injuries aims to water tightly close the globe and restore normal anatomy while avoiding further damage. This involves careful suturing and removal of disrupted lens, foreign bodies, and devitalized tissue. Post-operative care includes antibiotics and anti-inflammatory eye drops.