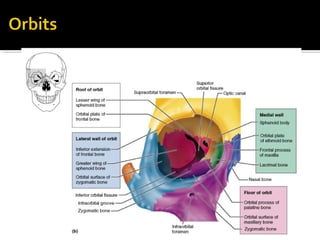
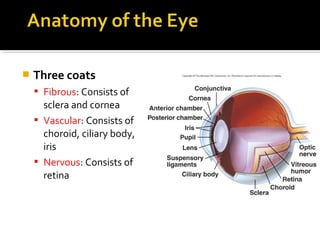
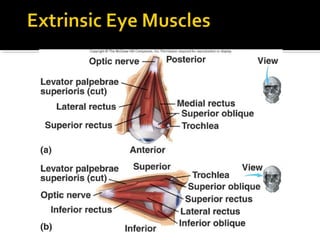
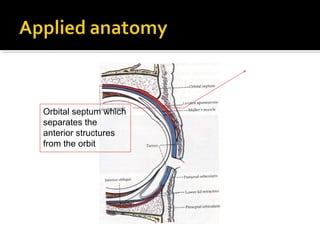
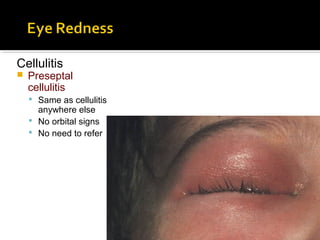
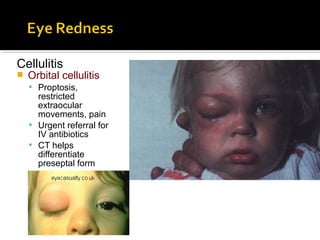
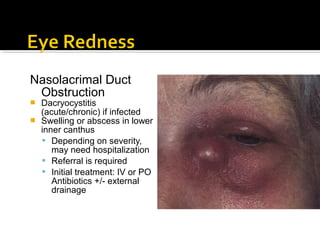
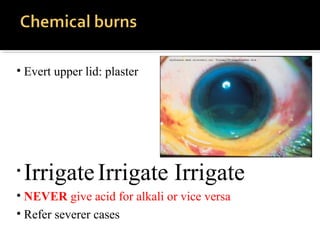
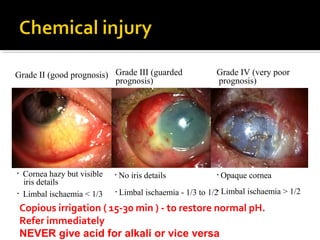
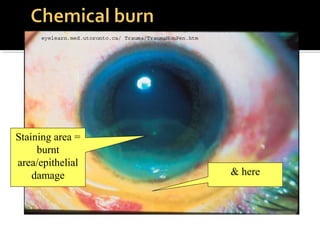
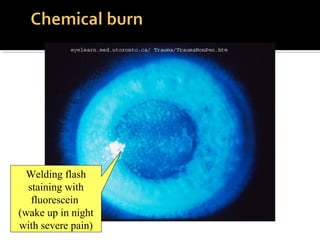
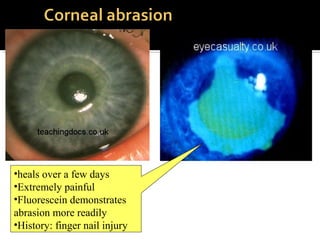
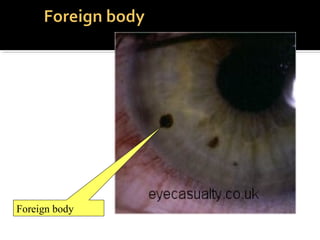
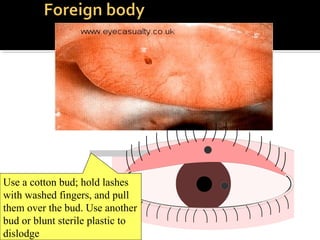
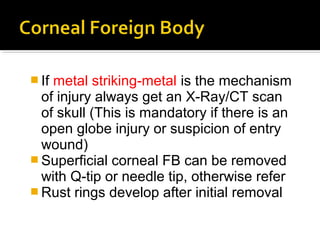
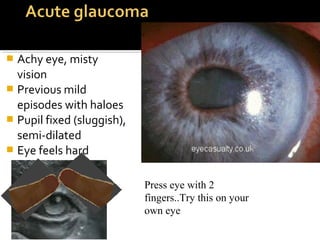
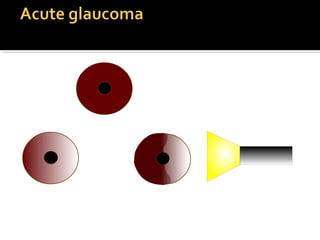
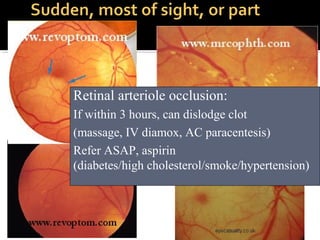
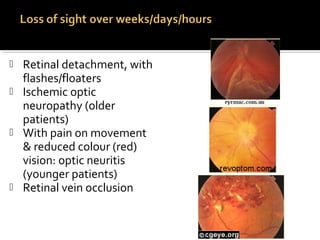
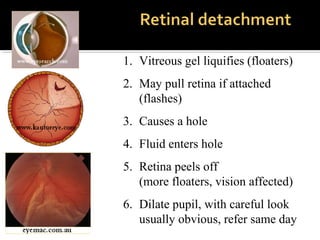
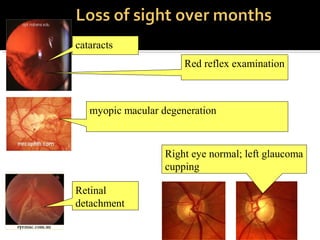
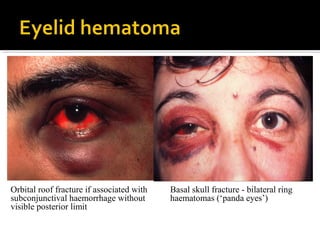
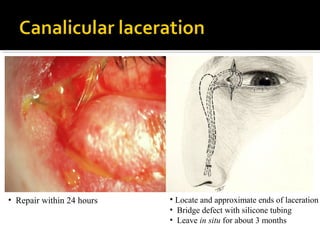
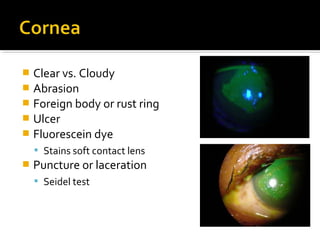
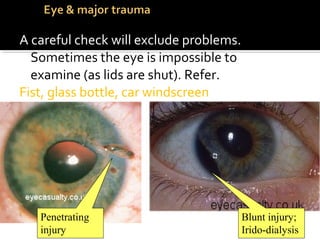
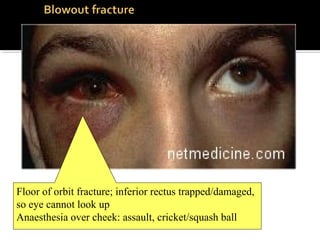
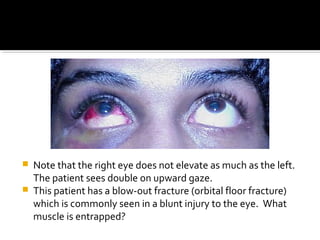
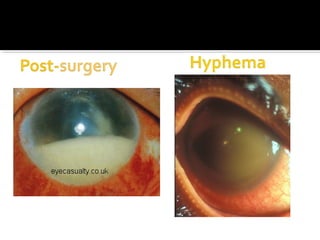
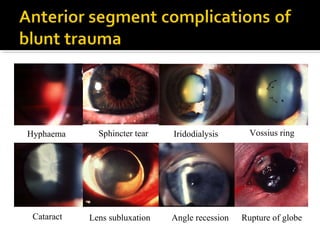
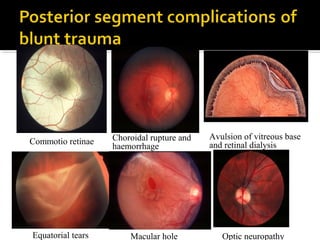
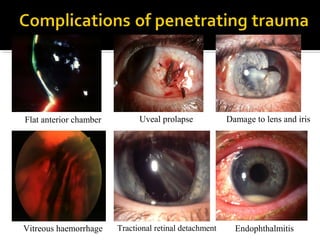
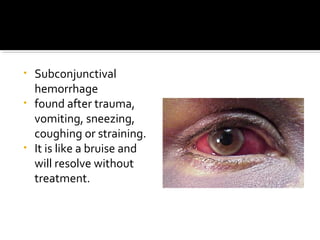
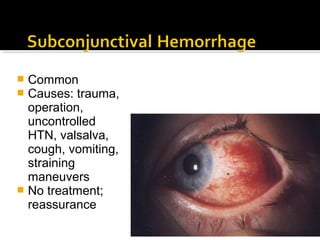
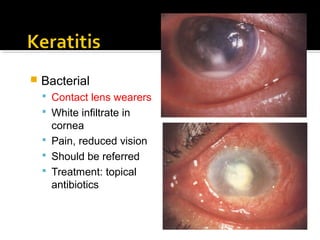
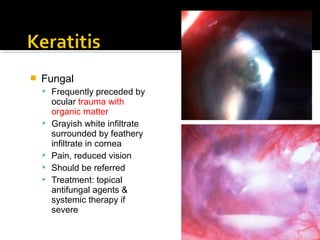
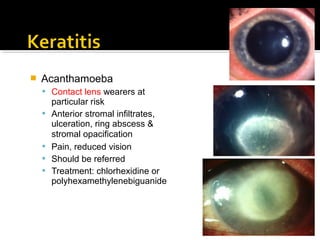
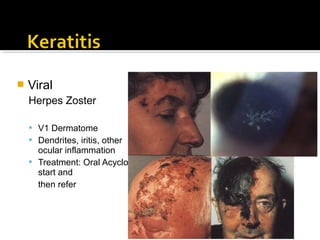
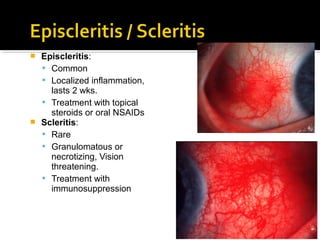
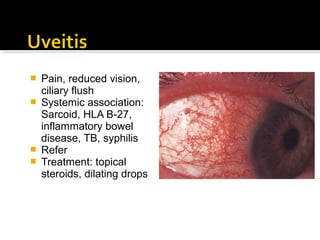
This document provides information on various eye conditions and injuries. It discusses eyelid hematomas and lacerations, orbital fractures, complications of blunt trauma, chemical injuries, eye anatomy, common eye problems, types of eye injuries and their signs, cellulitis, nasolacrimal duct obstruction, chemical burns grading and treatment, foreign bodies, open globe injuries, uveitis, glaucoma, retinal conditions, and various types of corneal ulcers and their causes and treatments.