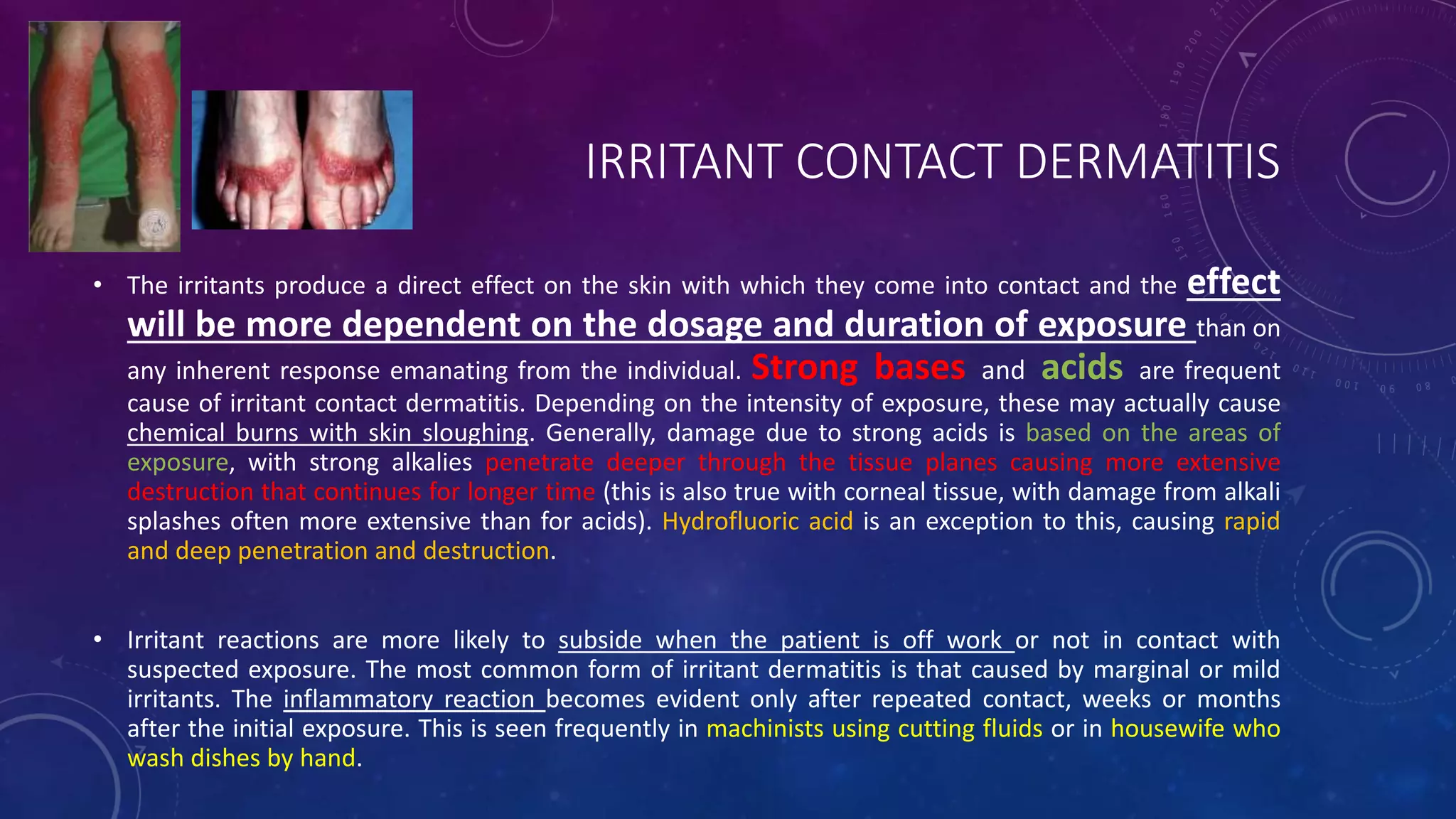
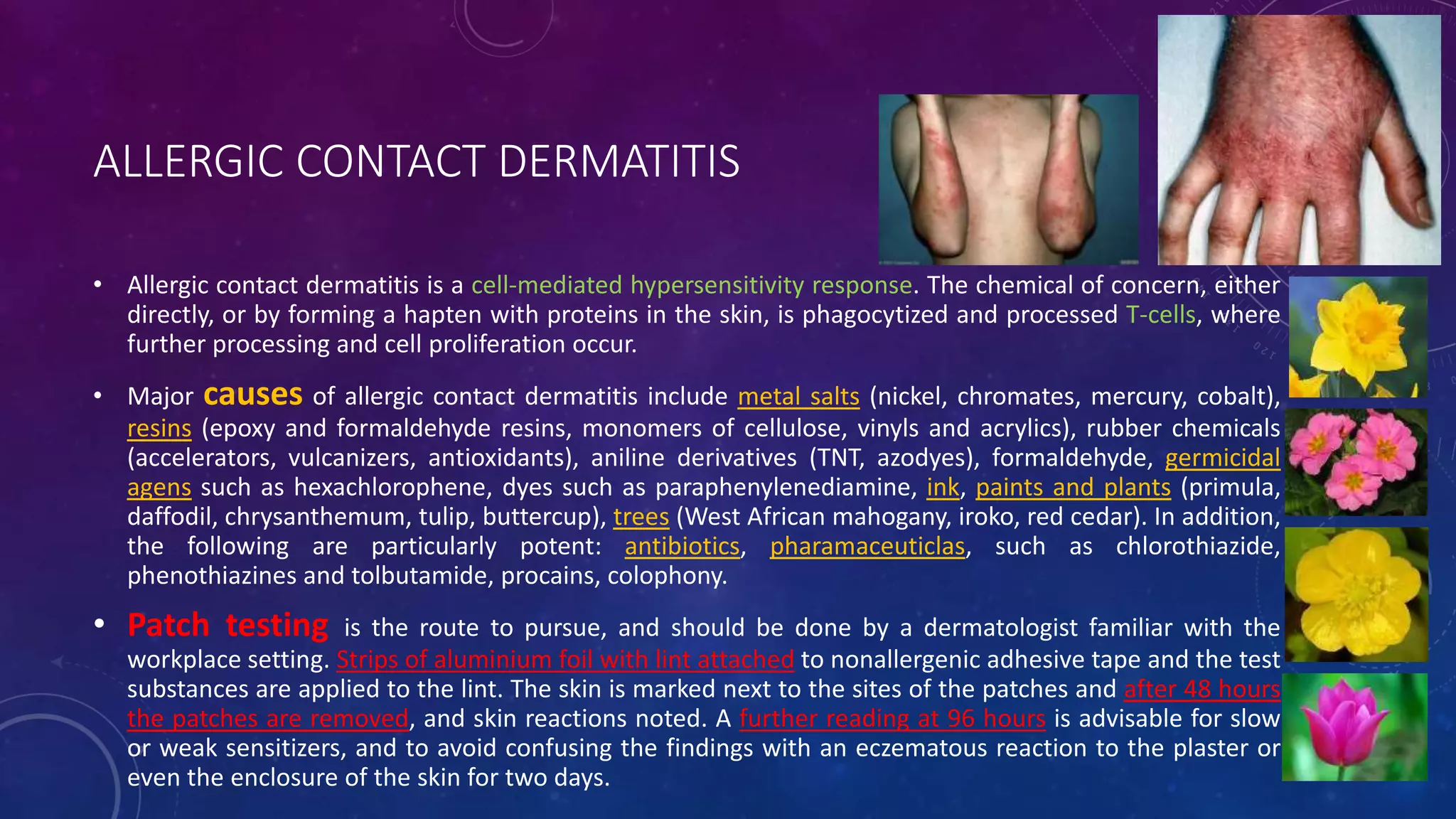
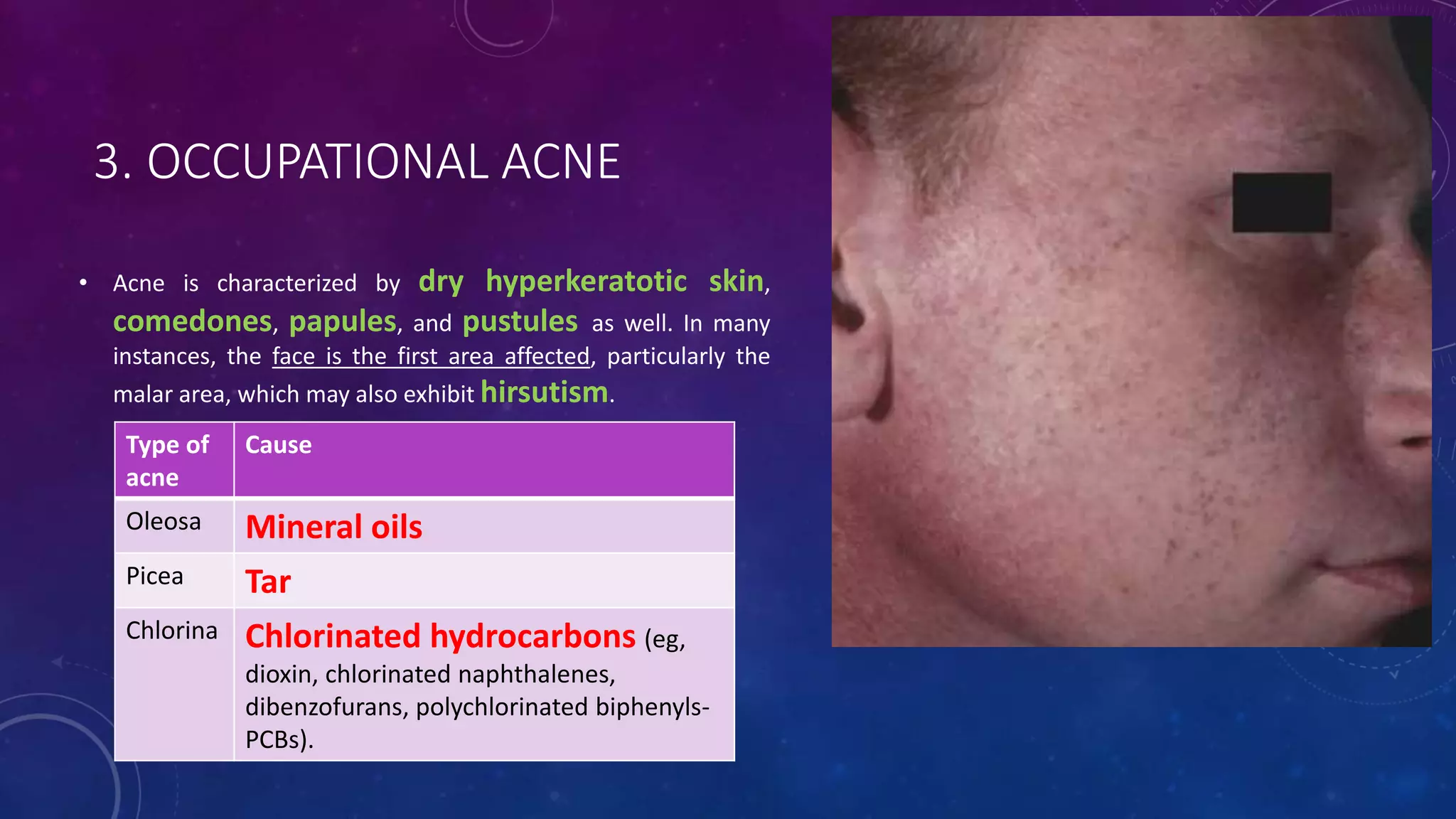
Occupational skin disorders represent 20% of all occupational diseases in the Czech Republic, with contact dermatitis being the most common type, attributed mainly to irritant and allergic reactions. Key industries linked to these skin diseases include leather goods, health professions, and agriculture, with diagnostic criteria focusing on exposure history and clinical manifestations. The document also discusses various specific skin conditions caused by occupational exposure, including infections, acne, and malignancies, highlighting the significance of protective measures and avoidance strategies.