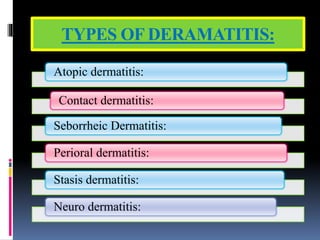
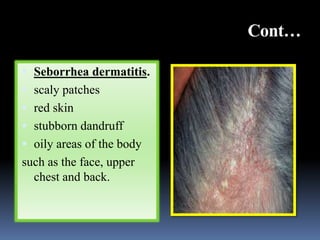
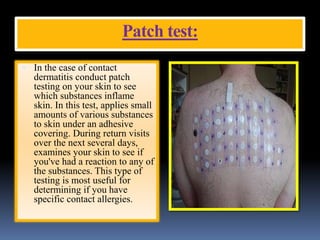
Dermatitis, or eczema, encompasses various skin conditions characterized by inflammation, itchiness, and rashes. Common types include atopic, contact, seborrheic, neuro, stasis, and perioral dermatitis, each with specific causes, symptoms, and management strategies. Effective treatment focuses on symptom relief and prevention, emphasizing skin care practices and potentially utilizing medications such as antihistamines and topical steroids.