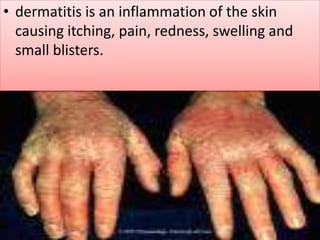
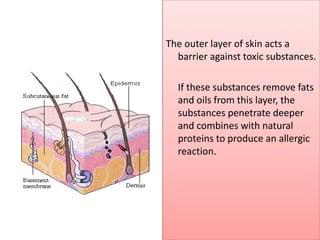
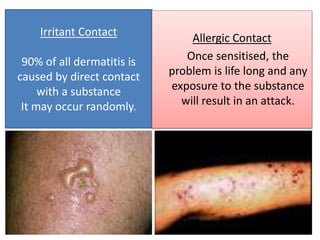
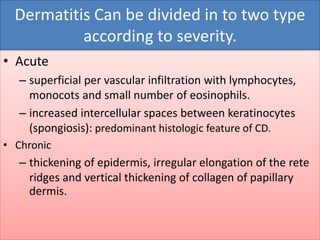
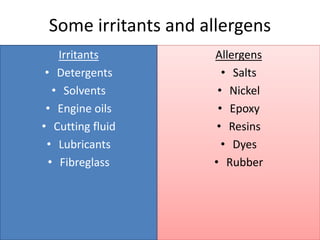
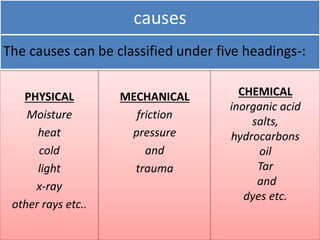
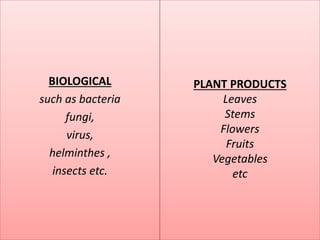
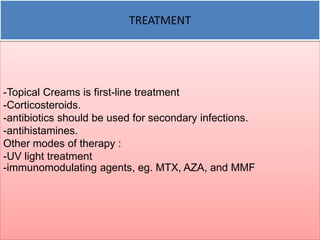
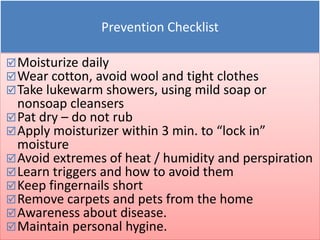
This presentation discusses occupational dermatitis, an inflammation of the skin caused by workplace exposures. Occupational dermatitis can be either irritant or allergic contact dermatitis. Irritant dermatitis occurs due to direct contact with irritating substances, while allergic dermatitis occurs through skin sensitization and exposure to specific allergens. The presentation outlines criteria for diagnosing occupational dermatitis and reviews common irritants and allergens seen in various workplaces. It also discusses the pathogenesis of dermatitis, types based on severity, treatment approaches including avoidance of triggers, and prevention through proper skin care and hygiene.