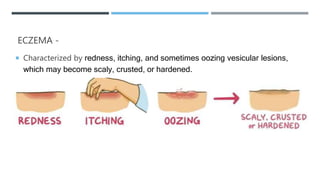
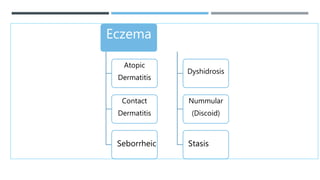
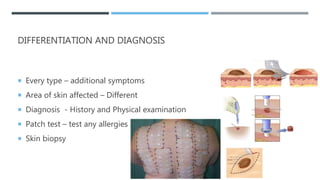
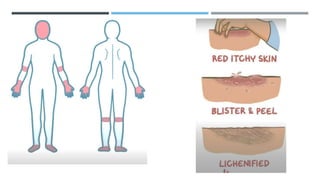
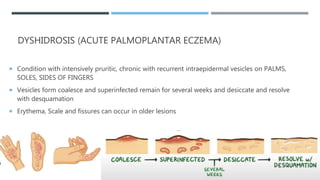
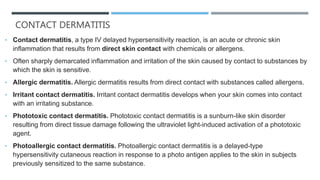
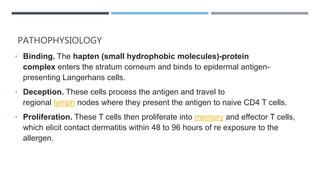
The document provides an overview of various types of eczema and dermatitis, including atopic dermatitis, contact dermatitis, and others, detailing their symptoms, diagnosis, and treatment options. It emphasizes the importance of identifying triggers, managing inflammation, and maintaining skin integrity through appropriate care. The document also highlights nursing assessments, interventions, and patient education necessary for effective management of these skin conditions.