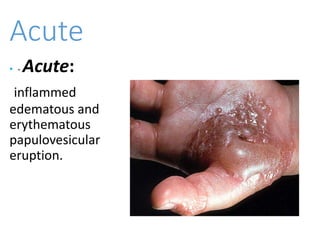
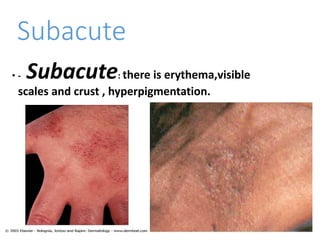
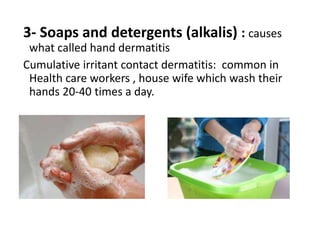
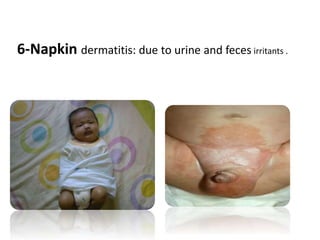
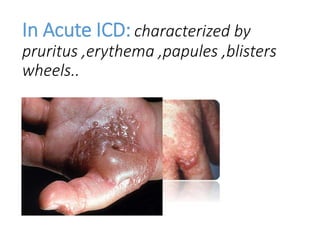
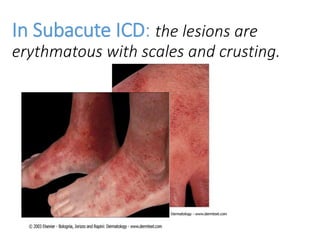
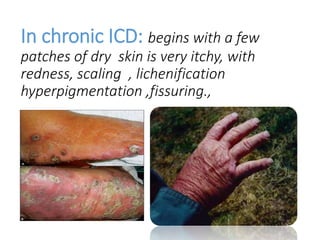
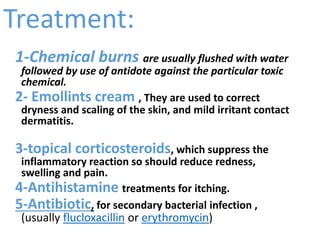
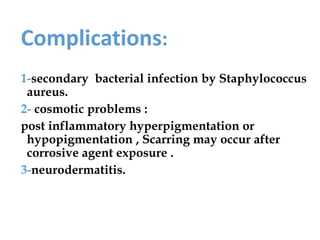
The document discusses dermatitis, particularly contact dermatitis, which is skin inflammation caused by irritants or allergens. It classifies dermatitis into etiological and clinical categories, outlining types, causes, and symptoms of irritant contact dermatitis, which can arise from both chemical and physical irritants. The document concludes with prevention strategies, treatment options, and potential complications related to contact dermatitis.