The document discusses burns, including:
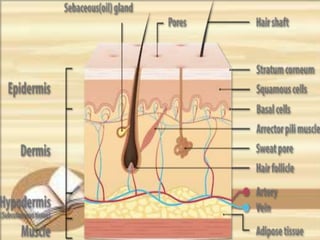
1. The structure of skin and how burns damage the epidermis and dermis layers.
2. The main causes of burns are thermal, chemical, inhalation, electric, and radiation burns.
3. Burn classification includes depth, extent, location, and patient risk factors which determine prognosis.
4. Burn management has three phases - emergent, acute, and rehabilitative - and the emergent phase focuses on airway management, IV fluids, wound care, drugs, and nutrition to stabilize the patient.