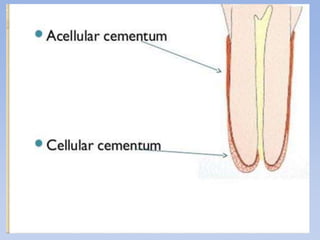
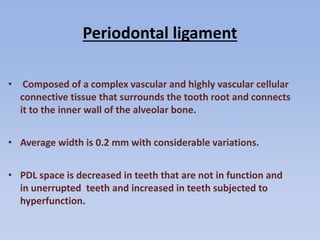
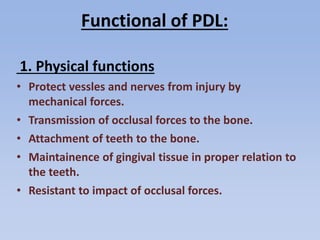
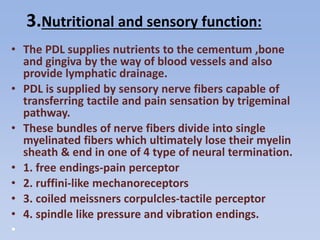
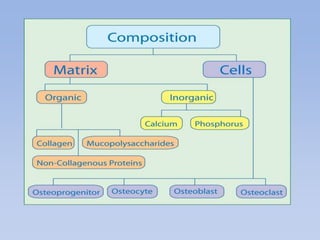
The periodontium is a specialized connective tissue that supports the tooth, comprising gingiva, cementum, periodontal ligament, and alveolar bone, each playing vital roles in maintaining oral health. Cementum, a calcified tissue that covers tooth roots, facilitates attachment to the alveolar bone and adapts to physical changes such as occlusal wear. The periodontal ligament connects teeth to the bone and undergoes constant remodeling, influencing tooth stability and health throughout life.