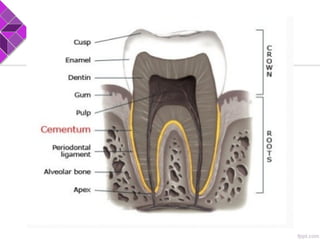
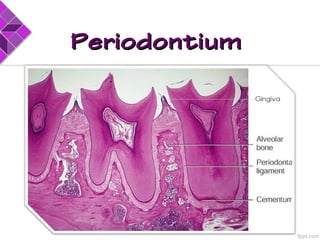
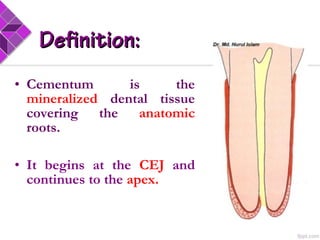
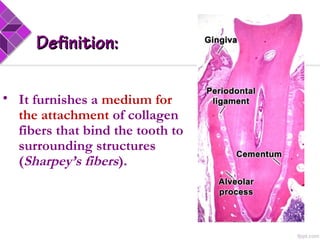
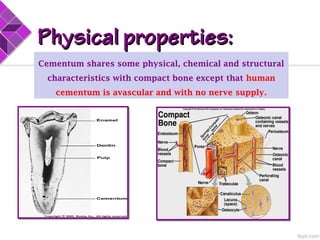
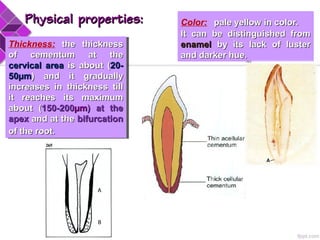
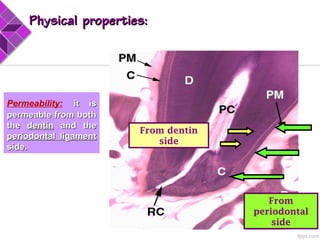
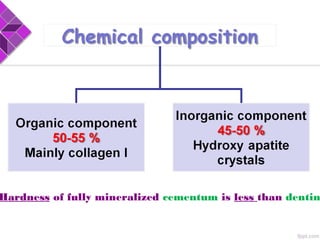
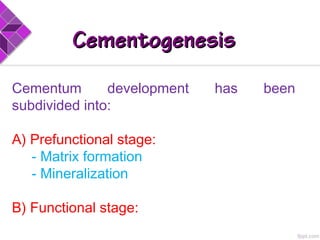
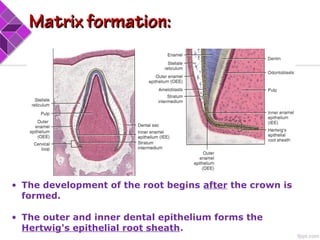
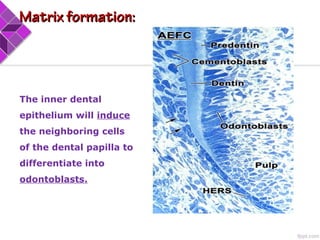
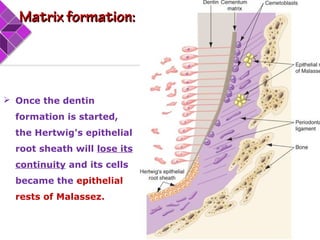
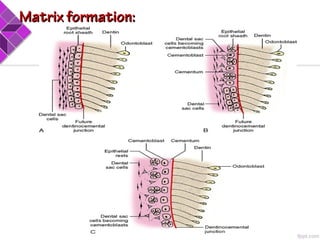
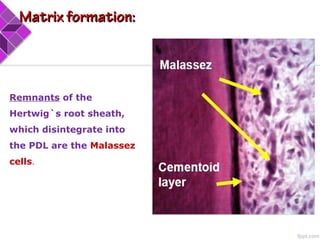
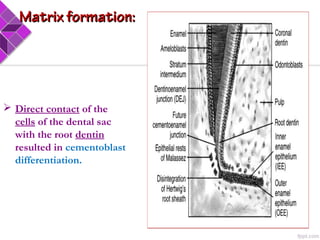
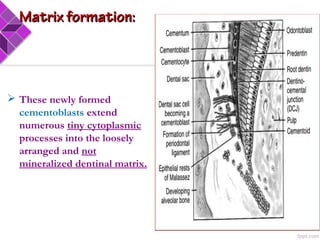
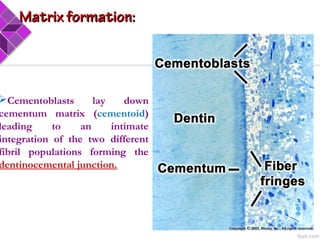
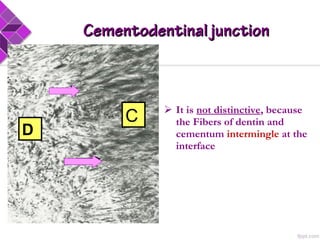
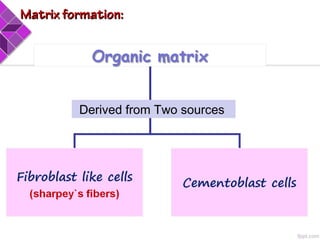
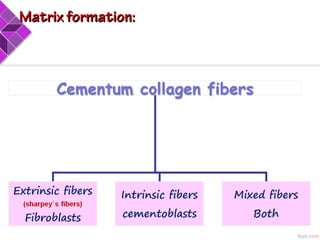
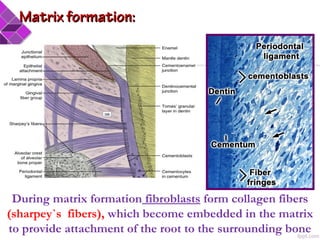
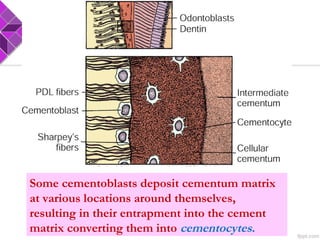
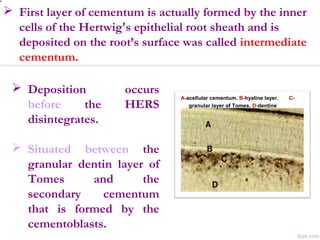
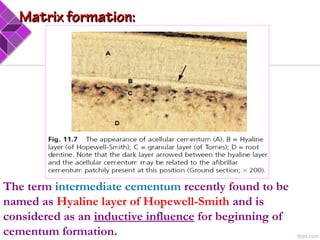
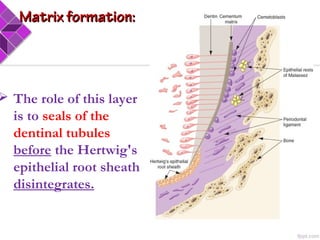
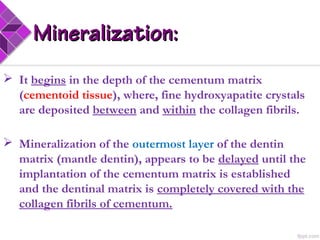
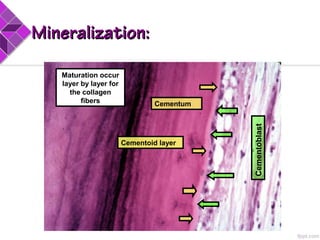
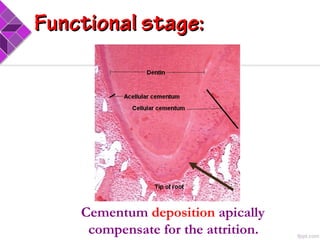
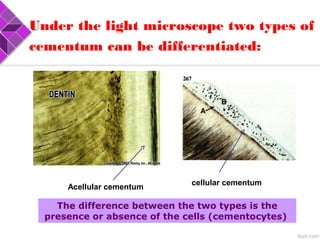
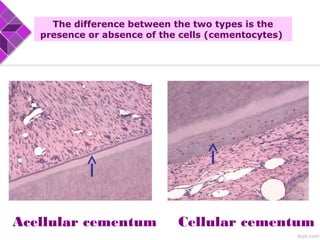
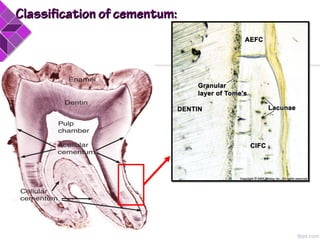
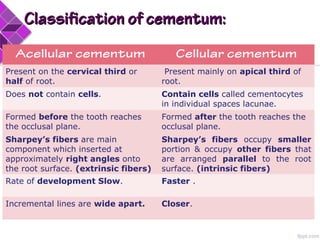
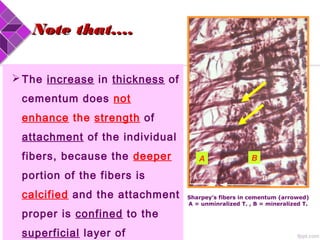
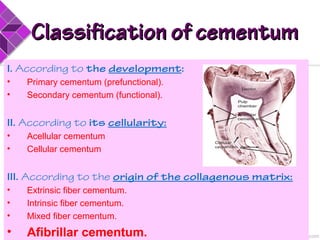
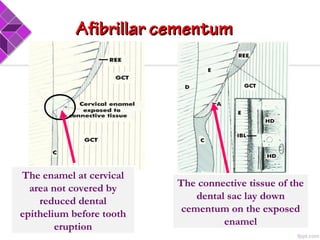
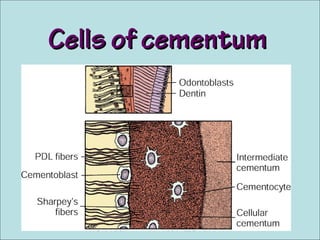
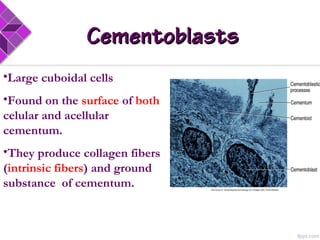
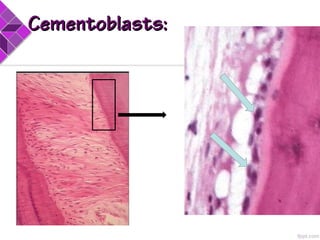
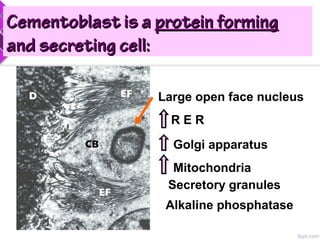
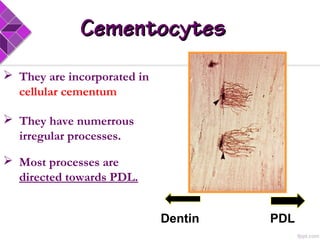
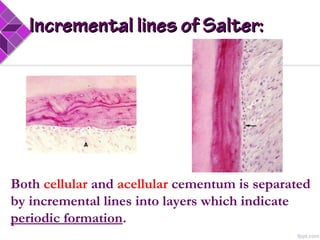
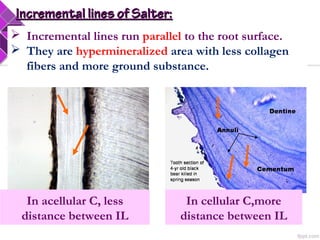
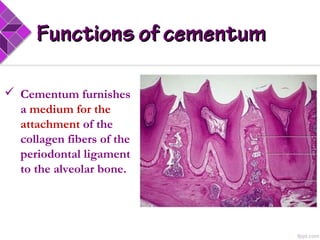
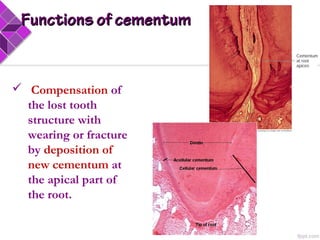
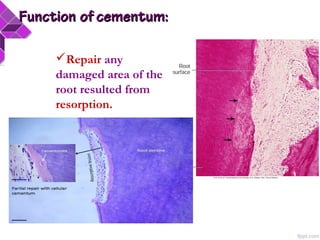
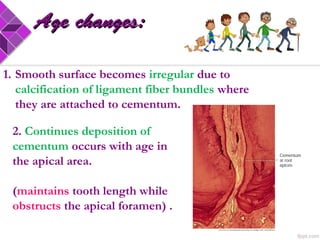
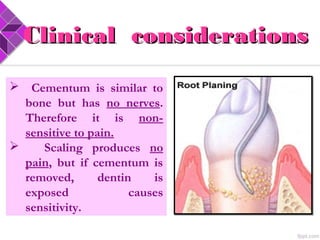
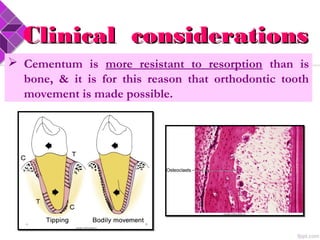
Cementum is the mineralized tissue covering dental roots. It begins at the cementoenamel junction and continues to the root apex. Cementum provides attachment for collagen fibers (Sharpey's fibers) that bind the tooth to surrounding structures. Cementum develops in two stages: the prefunctional stage involving matrix formation and mineralization, and the functional stage where cementum deposition continues throughout life in response to tooth movement and wear. Cementum comes in various forms classified by development, cellularity, and fiber origin and includes acellular, cellular, intrinsic and extrinsic fiber cementum.