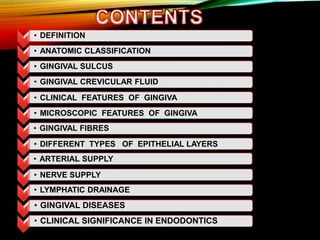
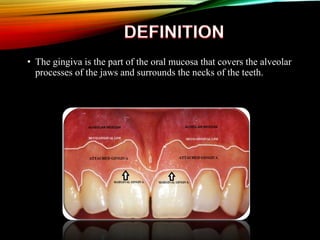
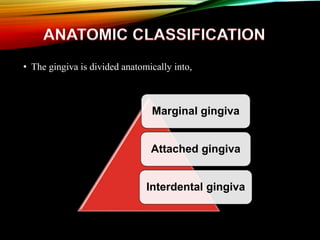
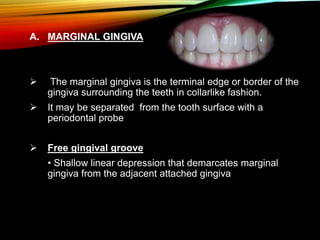
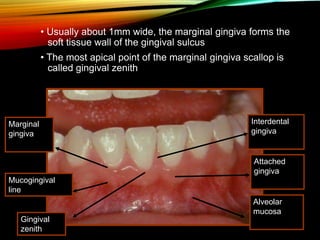
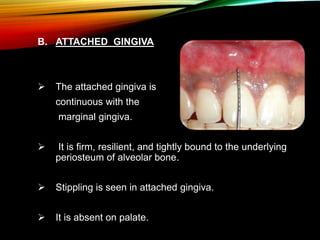
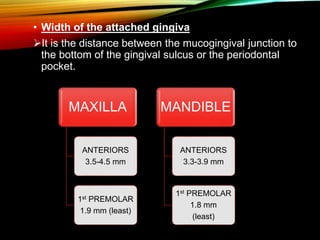
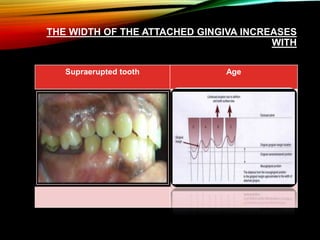
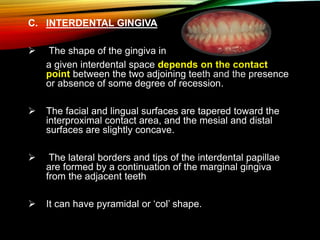
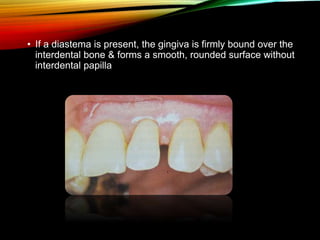
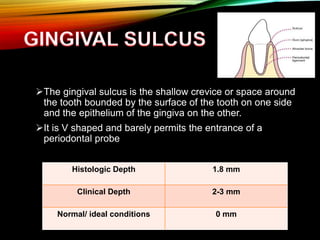
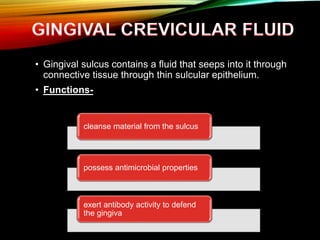
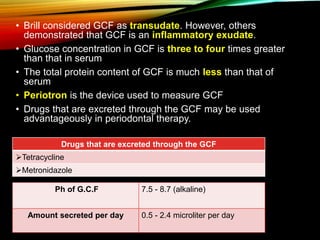
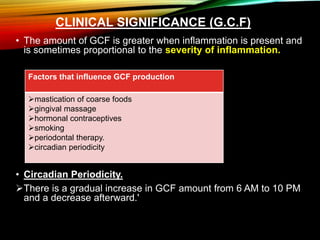
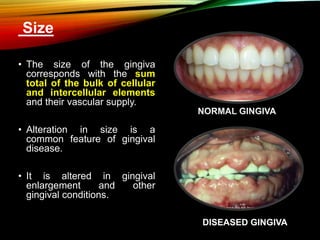
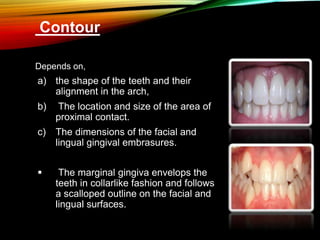
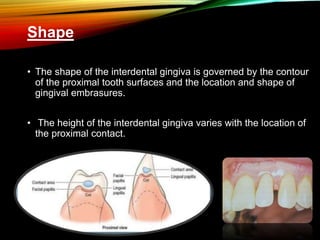
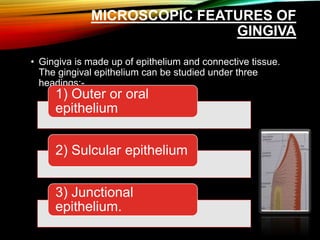
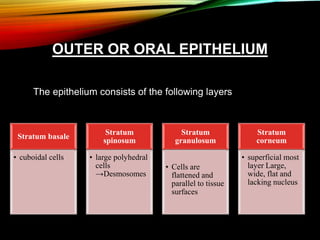
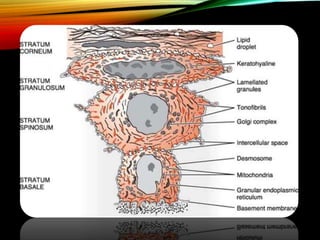
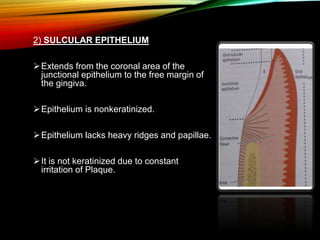
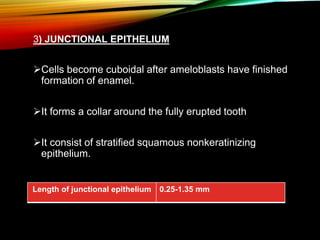
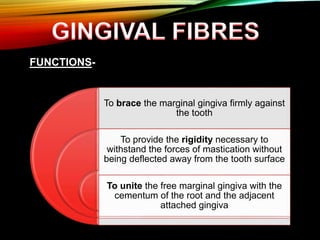
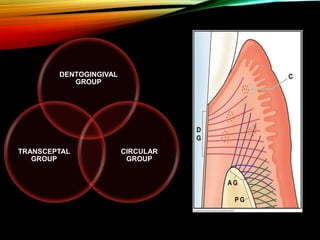
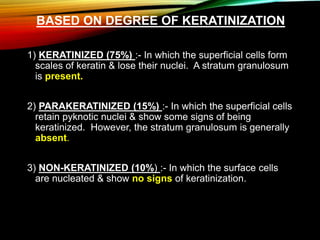
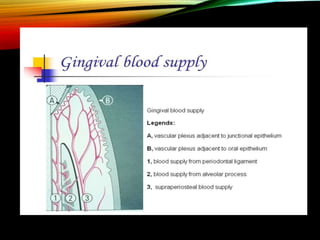
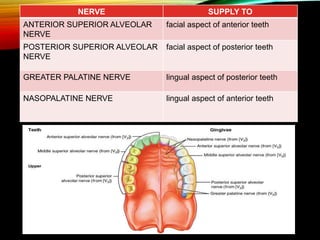
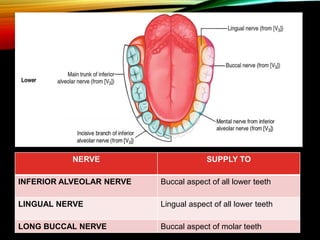
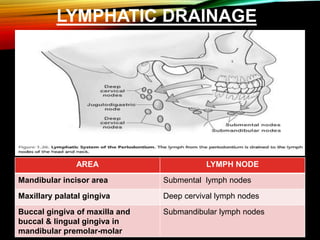
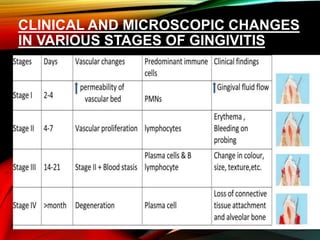
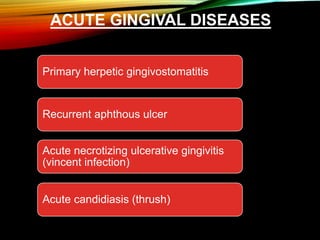
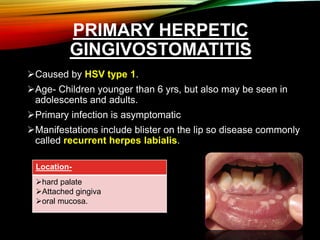
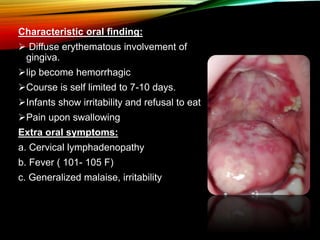
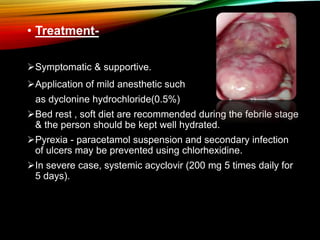
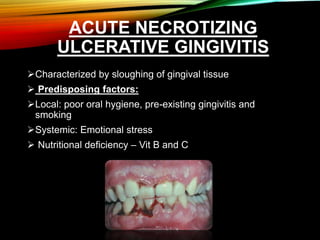
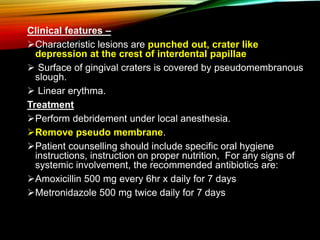
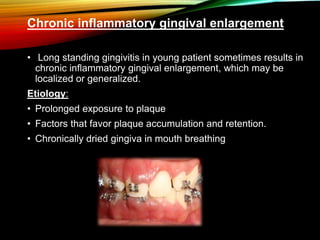
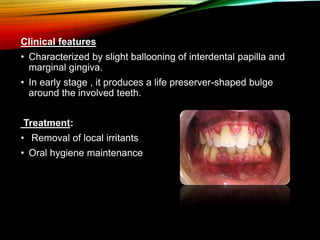
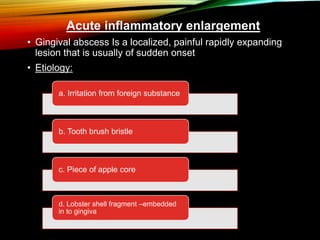
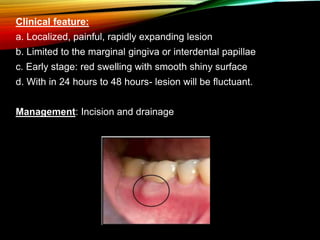
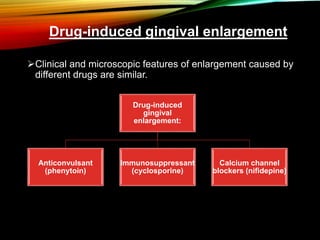
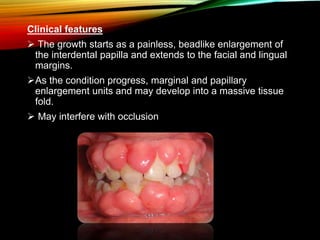
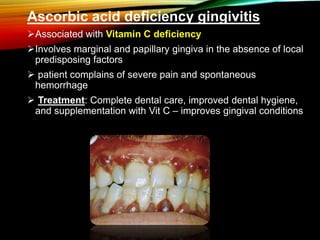
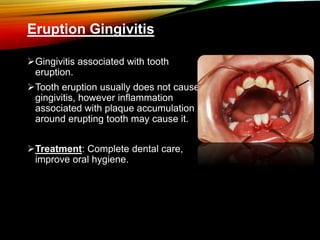
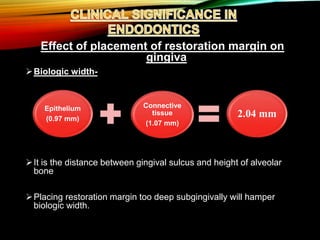
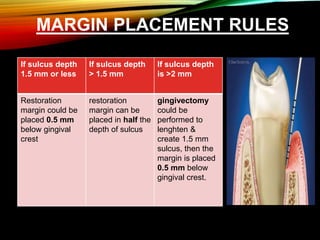
The document provides an extensive overview of gingival anatomy, classification, and clinical features including descriptions of marginal, attached, and interdental gingiva. It highlights the importance of gingival crevicular fluid (GCF), its function, factors influencing its production, and implications for periodontal health. Additionally, it discusses various gingival diseases, their clinical features, and treatments, along with the relationship between gingival health and dental restorations.