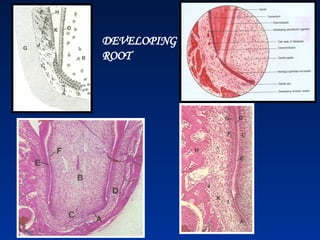
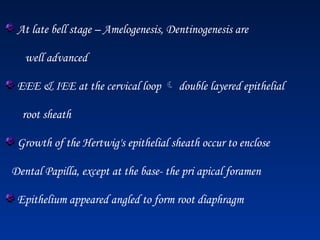
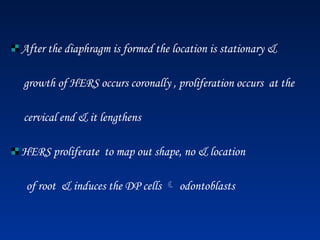
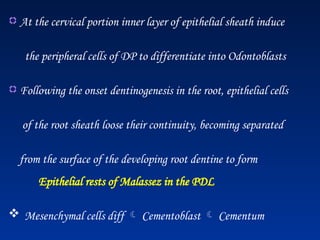
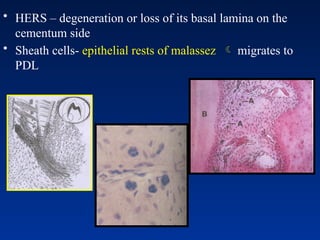
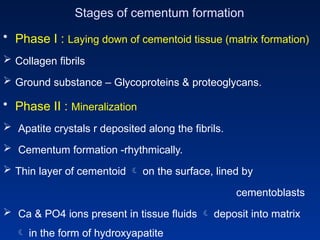
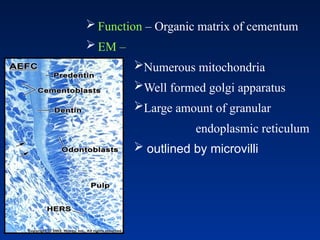
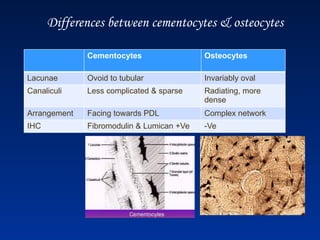
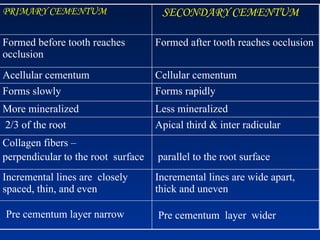
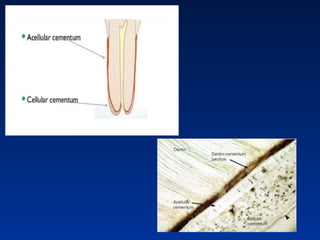
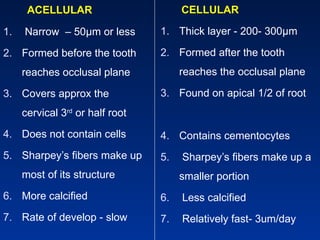
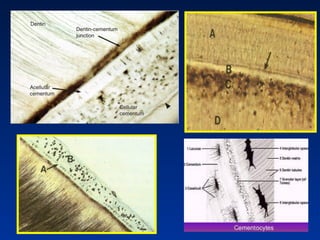
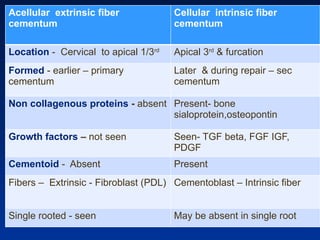
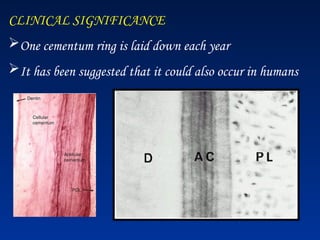
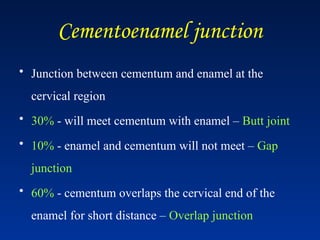
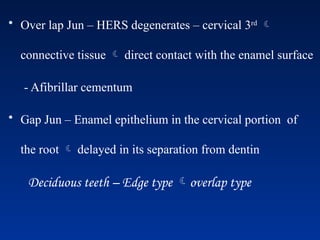
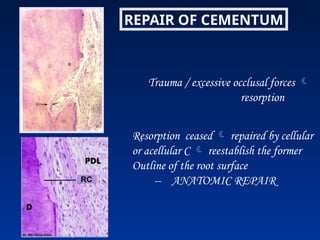
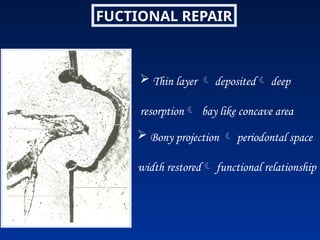
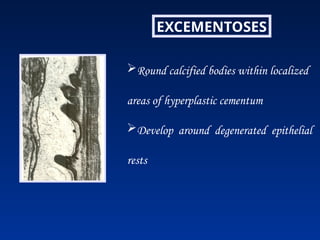
El documento detalla las etapas del desarrollo de las raíces dentales, centrándose en la formación del cemento y la dentina, así como la clasificación del cemento en primario y secundario. Se discuten las características físicas y químicas del cemento, incluyendo su composición orgánica e inorgánica, y su importancia en la función de anclaje y reparación dental. Además, se abordan aspectos clínicos como la hipercementosis y el movimiento ortodóntico de los dientes, junto con los cambios relacionados con la edad en el cemento.