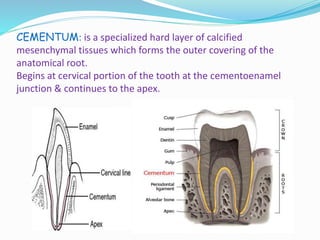
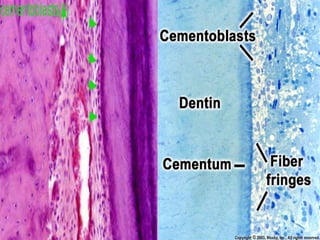
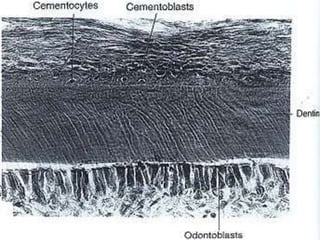
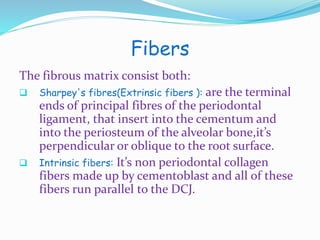
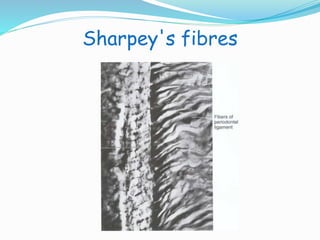
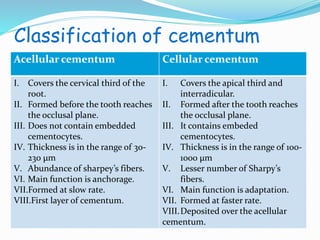
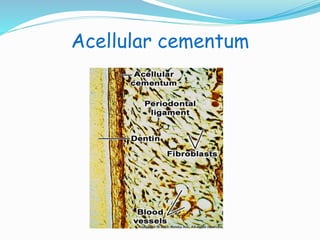
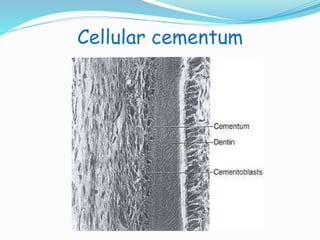
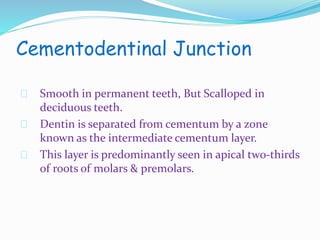
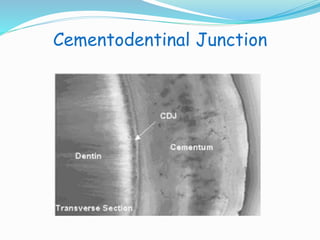
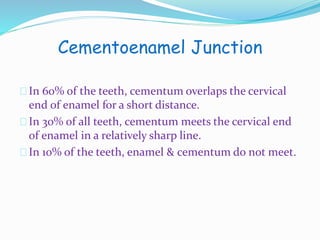
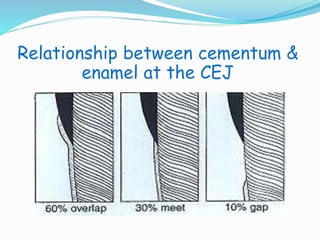
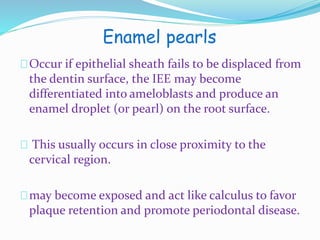
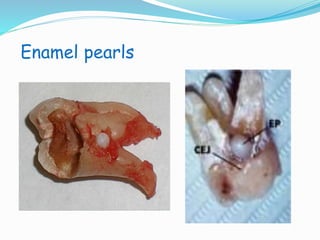
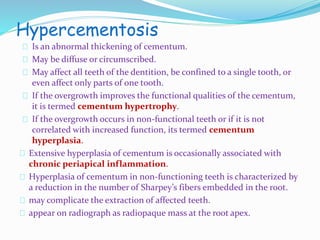
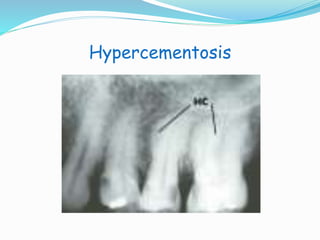
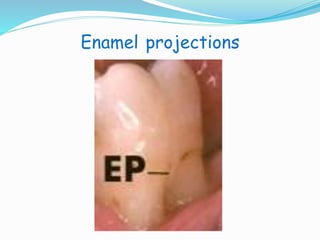
Cementum is the specialized mineralized tissue that covers the anatomical root of a tooth. It begins at the cementoenamel junction and continues along the root to the apex. Cementum functions to attach periodontal ligament collagen fibers to the root, serving as a medium for reattachment during repair. Cementum is thickest at the root apex and thinnest cervically. It is deposited throughout life by cementoblast cells and maintains periodontal ligament attachment through cementocyte cellular activity and Sharpey's fiber insertion. Developmental anomalies such as enamel pearls, hypercementosis, and cementicles can occur and impact periodontal health.