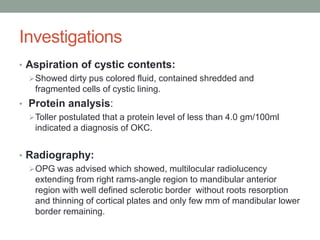
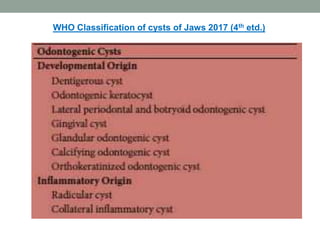
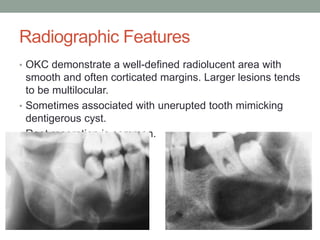
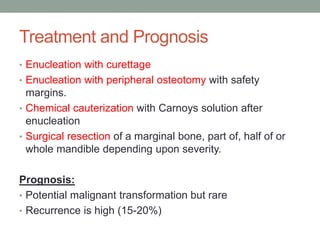
This case presentation describes a 74-year-old female patient with a swelling in the lower front region of her jaw. Radiographs and biopsy revealed an odontogenic keratocyst. Odontogenic keratocysts are developmental cysts that arise from cell rests of the dental lamina and have a high recurrence rate due to their thin lining. Treatment options considered for this patient's odontogenic keratocyst include curettage with or without peripheral osteotomy or segmental resection of the mandible.