Gingiva
- 1. DR.ANJU MATHEW K DEPARTMENT OF PERIODONTICS FIRST YEAR POSTGRADUATE
- 2. Introduction Gingiva Macroscopic anatomy Marginal gingiva Attached gingiva Width of attached gingiva Significance of attached gingiva Measurement of width of attached gingva Interdental gingiva,types Free gingival groove Gingival sulcus,development of gingival sulcus Gingival crevicular fluid Gingival biotype Microscopic features Oral epithelium Sulcular epithelium Junctional epithelium
- 3. Development of junctional epithelium Cells present in gingival epithelium Keratinisation,types Nonkeratinocytes Epithelium connective tissue interface Gingival connective tissue Gingival fibres-Function,Types Clinical features of gingiva and their correlation with microscopic features Color Contour Shape Consistency Surface texture Position Blood supply of gingiva Nerves Lymphatics References
- 4. The periodontium is a structural and functional group of tissues that together facilitate the anchorage of teeth in jaws There are four tissues that constitute the periodontium 1. Periodontal ligament 2. Alveolar bone 3. Gingiva 4. Cementum
- 6. CARANZA-Is the part of oral mucosa that covers the alveolar processes of jaw and surrounds the neck of the teeth. SCHROEDER-It is a combination of epithelium and connective tissue and is defined as that portion of oral mucous membrane, which in complete post eruptive dentition of a healthy young individual, surrounds and is attached to the teeth and the alveolar processes. GRANT-Is the part of mucous membrane attached to the teeth and the alveolar processes. LINDHE-Is that part of masticatory mucosa covering the alveolar processes and the cervical portions of teeth.
- 8. Oral mucosa Lining mucosa Specialized mucosa Masticatory mucosa Includes the gingiva and the covering of the hard palate Covers the dorsum of the tongue The remaining part
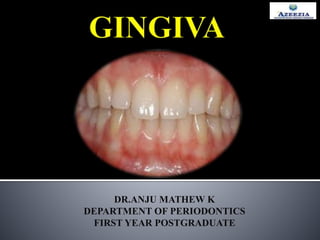
- 11. Attached gingiva Marginal gingiva Interdental gingiva
- 12. Also known as free gingiva It is coral pink, dull surface, firm in consistency It is the terminal edge or border of the gingiva surrounding the teeth like a collar. It is not fixed to the basal periosteum of alveolar bone . It is usually 1mm wide and forms the soft tissue wall of gingival sulcus
- 13. It is the distance between the mucogingival junction and the projection on the external surface of the bottom of the gingival sulcus or the periodontal pocket It is continous with the margnal gingiva It is firm reselient and tightly bound to the underlying tissues of the alveolar bone Mucogingival junction Important landmark between the coronally positioned attached gingiva and the apically placed alveolar mucosa Absent on the palatal gingiva of the maxilla due to an absence of a freely movable alveolar mucosa on the palate.
- 14. DIMENSIONS OF ATTACHED GINGIVA (ON FACIALASPECTS) REGION DIMENSION(mm) Maxillary incisor region 3.5-4.5 Mandibular incisor region 3.3-3.9 Maxillary 1st premolar 1.9 Mandibular 1st premolar Approx 1.8
- 16. The width of attached gingiva increases with age and supraerupted teeth Reduced/Absent attached gingiva may be due to: base of the pocket is close to the mucogingival line
- 17. Frenal/muscle attachments that encroach on pockets and pull them away from the tooth surface denudation of root surfaces
- 18. It gives support to the marginal gingiva It provides attachment or a solid base for the movable alveolar mucosa for the action of lips,cheeks,tongue It can withstand frictional and functional stresses of mastication and tooth brushing It acts as barrier for passage of inflammation It provides resistance to tensional stresses
- 19. Functionally by passive movement of lips and cheeks(Ochsenbein et al 1974,Cohen 1964) Measure the amount of width of attached gingiva using probe(substraction method) Staining method Roll method
- 20. Also known as interdental papilla Portion of gingiva located in the space between two adjacent teeth If a diastema is present the gingiva is firmly bound over the interdental bone and forms a smooth, rounded surface without interdental papilla
- 21. pyramidal col Where there is one papilla with its tip immediately beneath the contact point •Which represents as a depression that connects facial and a lingual papilla and conforms to the shape of interproximal contact •Non keratinized epithelium •Susceptible to inflammation and disease progression
- 22. Marginal gingiva is separated from an attached gingiva by a shallow line called as free gingival groove Located corresponding to the level of cementoenamel junction(CEJ) Present in only about 30%-40% Free Gingival Groove
- 23. Shallow space/crevice around the tooth bounded by the surface of the tooth on one side and epithelium lining the free margin of the gingiva on the other side V shaped and rarely permits the entrance of a periodontal probe. The probing depth 2-3mm
- 25. After the enamel formation is complete , the enamel is covered with REE(reduced enamel epithelium),which is attached to the tooth by a basal lamina & hemidesmosomes When tooth penetrates oral mucosa,the REE unites with oral mucosa and transformed into JE JE proceeds in an apical direction ,forming a shallow groove,the gingival sulcus between circumference of tooth & gingiva that encircles the newly erupted tip of the crown Gingival sulcus deepens as a result of seperaton of the REE from actively erupting tooth & JE attains its position at CEJ of fully erupted tooth
- 27. The gingival sulcus contains a fluid that seeps into it from the gingival connective tissue through the thin sulcular epithelium Inflammatory exudate derived from the periodontal tissues Found in sulcus/periodontal pocket between tooth and marginal gingiva Composed of serum and locally generated materials such as tissue breakdown poducts,inflammatory mediators and antibodies directed against dental plaque bacteria Plays special part in maintaining the structure of junctional epithelium and the antimicrobial defense of periodontium In healthy sulcus,the amount of GCF is very less During inflammation ,the GCF flow increases . The increasd GCF flow contributes to host defense by flushing bacterial colonies and their metabolites away from the sulcus The man route of gcf diffusion is through the basement menbrane and then through the junctional epithelium into the sulcus
- 28. Significance of gingival crevicular fluid 1. To assess the severity of gingival diseases, the effectiveness of periodontal therapy and oral hygiene, the healing following gingival surgery, and the effectiveness of oral hygiene 2. To evaluate the rate of local destruction, to assess the permeability of junctional and sulcular epithelium, and to assess the relationship between periodontal and systemic diseases Factors stimulating gingival crevicular fluid flow 1. Gingival inflammation, mastication of coarse food, pocket depth, intracrevicular scraping, scaling, and histamine topical application 2. Enzymes and sex hormones: female sex hormones increases the gingival fluid flow 3. Circadian periodicity: gradual increase in gingival fluid amount from 6 AM to 10PM 4. Post- periodontal surgery, restoratve procedure, strip placement, mobility, increased body temperature and salivary contamination 5. Ovulation ,hormonal contraceptives and smoking
- 29. Method of collection 1. Absorbing paper strips 2. Preweighed twisted threads 3. Micropipettes 4. Crevicular washings Composition of GCF 1. Celluar elements 1. Epithelial cells 2. Leukocytes 3. Bacteria 2. Electrolytes 1. Na:K 2. Flouride,calcium,iodine and phosphorous 3. Organic compounds 1. Carbhohydrates 2. Proteins 3. Immunoglobulis 4. Complement 5. Cytokines 6. Metabolic and bacterial products
- 31. The thickness of the gingiva in the faciopalatal /faciolingual dimension. Reduced gingival thickness is one of the factors that can cause periodontal attachment loss and marginal tissue recession The term periodontal biotype introduced by Seibert and Lindhe categrized the gingiva into “thick flat”and “thin scalloped”biotypes Thick biotype broad zone of keratinized tissue flat gingival contour which indicates thick underlying bony architecture More resilient to any inflammation or trauma Thin biotype Thin band of the keratinized tissue Scalloped gingival contour , which indicates thin bony architecture More sensitive to inflammation or trauma
- 34. Histological examination of gingiva exhibited following structures: Gingival epithelium Epithelium connective tissue interface Gingival connective tissue or lamina propria
- 36. Called as outer epithelium Keratinized stratified squamous type epithelium It covers the crest and outer surface of marginal gingiva and surface of the attached gingiva The oral epithelium consists of following types of cellular layers Oral Epithelum
- 37. 1. Stratum basale: Cells either cylindrical or cuboidal Found immediately next to connective tissue and separated by a basement membrane Germinative layer, hence it can divide When two daughter cells are formed by cell division, an adjacent older basal cell is pushed into the spinous cell layer and starts as a keratinocyte to transverse the epithelium 2. Stratum spinosum: prickle cell layer Polyhedral cells with short cytoplasmic processes are present Uppermost cells from this layer contain granules called as keratinosomes or odland bodies 3. Stratum granulosm: Cells are flattened in plane parallel to the gingival surface Keratohylain granules associated with keratin formation round in shape and appear within in cytoplasam of the cell 4. Stratum corneum: Closely packed flattened cells, lost nuclei. Cells are densely packed with tonofilaments Rounded bodies probably representing lipid droplets appear within the cytopasam of the cell
- 39. Nonkeratinized stratified squamous epithelium Lines the gingival sulcus Apically bounded by the junctional epithelium,coronally it meets the outer gingival epithelium at the height of gingival margin Lacks granulosum , corneum strata,K1,K2 and K10 to K12 cytokeratins It contains K4 and K13 so called esophageal type cytokeratins Also express K19 Does not contain merkel cells Lack of keratinization makes this area particularly susceptible to influences from microorganism It has the potential to keratinize if It is reflected and exposed to the oral cavity Bacterial flora of the sulcus is totally eliminated Act as semipermeable membrane, through which injurious bacterial products pass into the gingival and tissue fluid from gingiva seeps into the sulcus No rete pegs
- 40. Collar like band of stratified squamous non keratinizing epithelium 3 to 4 layers thick in early life ,the number of layers increase with age to 10 or even 20 layers The cells can be grouped in two strata: Basal layer: Facing the connective tissue Suprabasal layer: Extending to the tooth surface The length of juntional epithelium 0.25 to 1.35 mm The junctional epithelium is formed by the confluence of the oral epithelium and the reduced enamel epithelium during tooth eruption K19 and K5,K14-Stratification-specific cytokeratins It exhibits lower glycolytic enzyme, lacks acid phosphatase activity
- 41. The junctional epithelium is attached to the tooth surface- internal basal lamina It is attached to the gingival connective- external basal lamina THE DENTOGINGIVAL UNIT: The attachment of the junctional epithelium to the tooth is reinforced by the gingival fibres, which brace the marginal gingiva against the tooth surface For this reason the juctional epithelium and the gingival fibers are considered together as a functional unit
- 42. Hypothesis given to explain mode of attachment of epithelium to tooth surface 1.GOTTLIEB 1921:gingiva is organically united to surface of enamel. He termed it as epithelial attachment 2.ORBAN1953:stated that the separation of the epithelial attachment cells from the tooth surface involved preparatory degenerative changes in the epithelium 3.WAERHAUG 1960:presented a concept of epithelial cuff, he concluded that gingival tissues are closely adapted but not organically united 3.SCHROEDER AND LISGARTEN 1971: Based on transmission electron microscopic studies,they proved the existence of a hemidesmosomal basement lamina attachment between the tooth and the cells of the so called cells of epithelial attachment
- 43. Firmly attached to the tooth surface forming an epithelial barrier against plaque bacteria Allows access of gingival fluid, inflammatory cells, and components of the immunologic host defense to the gingival margin Exhibits rapid turnover contributing t the host-parasite equilibrium and the rapid repair of damaged tissue Have an endocytic capacity equal to that of macrophages and nuetrophils and that this activity may be protective in nature
- 44. As an erupting tooth approaches the oral epithelium, the enamel epithelium rapidly proliferates forming the thick reduced enamel epithelium. As the crown erupts further, the reduced enamel epithelium overlying the enamel fuses with the oral epithelium, undergoes transformation and establishes the dentogingival junction forming the junctional epithelium cells
- 45. The junctional epithelium maintains a direct attachment to the tooth surface. During eruption, contact is established between the reduced enamel epithelium and oral gingival epithelium. Epithelial cells of junctional epithelium contact with the tooth surface by internal basal lamina and separated from the connective tissue by the external basal lamina
- 47. DIFFRENCE BETWEEN ORAL,SULCULAR AND JUNCTIONAL EPITHELIUM ORAL SULCULAR JUNCTIONAL KERATINIZATION Keratinised Non keratinised Non keratinised RETE PEGS Present Absent Absent STRATUM GRANULOMAAND CORNEUM Present Lacking Lacking MERKEL CELLS Present Absent Absent LANGERHANS CELLS Present Few Absent TYPE IV COLLAGEN IN BASAL LAMINA Present Absent Absent TIGHT JUNCTIONS More Few Few ACID PHOSPHATASE ACTIVITY Present Lacking Lacking GLYCOLYTIC ENZYME ACTIVITY High Lower Lower INTERCELLULAR SPACE Narrower Narrower Wider
- 48. Cells present namely are keratinocytes and non keratinocytes Keratinocytes: 90% of the total gingival cell population Orginate from the ectodermal germlayer It have nucleus,cytosol,ribosome and golgi apparatus It have melanosomes,which are the pigment bearing granules present with in these cells only and not in the other cells of the periodontium
- 49. The main function of gingival epithelium is to protect the deep structures,this is achieved by proliferation and diffrentiation of the keratinocytes Proliferation :it takes place by mitosis in the basal layer Diffrentiation:involves process of keratinization ,which consists of progressions of biochemical and morphologic events that occur in basal layer The main morphologic changes are: Progressive flattening of cells Increase in tonofilaments Intercellular junctions coupled to the production of keratohyalin granules Disappearence of nucleus
- 50. Expression and synthesis of keratin proteins in the basal layer of cell,their chemical compositon in the upper layer and their interaction with keratohylin granules and formatin of filamentous matrix structure in the interior of corneocyte and strengtening of the envelope. Also known as CORNIFICATION -The journal of western society of periodontology,1979
- 51. Three types of surface keratinization can occur in the gingival epithelium 1.Orthokeratinization 2.Parakeratinization 3.Nonkeratinization
- 52. Complete keratinization of superficial horny layer No nuclei in stratum corneal layer Well defined stratum granulosum Few areas of outer gingival epithelium
- 53. Intermediate stage of keratinization Most prevalent surface area of the gingival epithelium Stratum cornea retains pyknotic nuclei Keratohyalin granules are disperesed rather than giving rise to a stratum granulosum
- 54. • Viable nuclei in superficial layers • Has neither granulosum nor cornea strata • Layers of non keratinized epithelium Stratum superficiale Stratum intermedia Stratum basale
- 55. The various nonkeratinocytes or clear cells are langerhans cells,merkel cells and melanocytes Melanocytes Melanocytes are dendritic cells located in the basal and spinous layers of the gingival epithelium . They synthesize melanin in organelles called premelanosomes or melanosomes . These contain tyrosinase, which hydroxylates tyrosine to dihydroxy phenylalanine (dopa), which in turn is progressively converted to melanin. Melanin granules are phagocytosed and contained within other cells of the epithelium and connective tissue, called melanophages or melanophores.
- 56. Langerhans Cells Langerhans cells are dendritic cells located among keratinocytes at all suprabasal levels . They belong to the mononuclear phagocyte system (reticuloendothelial system) as modified monocytes derived from the bone marrow. They contain elongated granules and are considered macrophages with possible antigenic properties. Langerhans cells have an important role in the immune reaction as antigen-presenting cells for lymphocytes. They contain g-specific granules (Birbecks' granules) and have marked adenosine triphosphatase activity. They are found in oral epithelium of normal gingival and in smaller amounts in the sulcular epithelium; they are probably absent from the junctional epithelium of normal gingiva. It stains with: Gold chloride, ATPase, Immuno florescent markers .
- 57. Merkel Cell Merkel cells are located in the deeper layers of the epithelium, harbor nerve endings, and are connected to adjacent cells by desmosomes. They have been identified as tactile preceptors. Stained by PAS
- 58. Boundary where epithelial tissue meets with connective tissue. Deep extensions of an epithelium that reach down into connective tissue are called epithelial ridges or retepegs Finger like extensions of connective tissue that extend up into the epithelium are called as connective tissue papillae Epithelial connective tissue interface is composed of lamina lucida and lamina densa Lamina lucida is an electrolucent zone of 25-45nm width and composed of glycoprotein laminin Laminin densa is an electrodense zone of 40-60nm where type IV collagen is present
- 60. TIGHT JUNCTION/ZONAE OCCLUDENS: Formed by the fusion of external leaflets of adjacent cell membranes ADHESIVE JUNCTIONS: 1. Cell to cell: zonula adherens desmosomes:most common type of junction 2. Cell to matrix focal adhesions hemidesmosomes COMMUNICATING (GAP) JUNCTIONS: Intercellular pipes/channels bridge both adjacent membranes and intercellur space Intercelluar space in gap junction is approx 3nm Majority pathway for direct intercellular communication
- 62. Also called as lamina propria Composed of 1. Ground substance 2. Cells 3. Gingival fibres Layers of connective tissue 1. Papillary layer 2. Reticular layer
- 63. Fills space between fibres and cells Amorphous High water content Composed of: Proteoglycans: Decorin Biglycan Versican Heparin sulfate proteoglycans and syndecans CD44 Glycoprotein: Fibronectin Laminin
- 64. The different types of cells present in the connective tissue are o Fibroblasts oPolymorphonuclear cells oLymphocytes and Plasma cells oMonocytes and macrophages oMast cells oOsteoblast and Osteoclasts oCementoblasts and cementoclasts
- 65. Most abundant cells They make 65% of the total cell volume of the gingival connective tissue Derived from undifferentiated progenitor mesenchmal cells, that are present in the follicle Elongated or spindle shaped cells Have prominent golgi apparatus, rough endoplasmic reticulum, mitochondria,vacoules and vesciles It synthesize and secrete various cytokines, growth factors and metabolic products All these play a vital role in the development, maintanence and repair of gingival connective tissue. Responsible for the resorption of collagen fibres ,thus playing important role in collagen homeostasis.
- 66. The connective tissue fibres are produced by the fibroblasts and can be divided into Collagen fibres Reticulin fibres Oxytalan fibres Elastic fibres Collagen fibre types: Type I,III,IV,V,VI Type I: It predominates,gives tensile strength Type III: 1.fetal collagen 2.important in the early phases of wound healing. 3.partly responsible for the maintanence of space in healing matrix Type IV: present in lamina densa layer of the basement membrane of the epithelium. Type VI 1.distributed with the elastin fibres along the blood vessels. 2.impart rigidity required to maintain the elastic blood vessel wall from undergoing permanent deformation. 3.acts as anchoring fibrils and helps to reinforce epithelial attachment to the underlying connective tissue
- 67. To brace the marginal gingiva firmly against tooth To provide rigidity to necessary to withstand the forces of mastication without being deflected away from the tooth surface To unite the free marginal gingiva with the cementum of the root and the adjacent attached gingiva
- 68. There is a specific of orientation and organization of the collagen fibre bundles in the gingival connective tissue, also referred to as fiber apparatus of gingiva. These are named according to their location, origin and insertion
- 69. Name of fiber group Origin and orientation Supposed function Principal groups Dentogingival From cementum, splay laterally into lamina propria Provide gingival support Alveologingival From periosteum of the alveolar crest, splay coronally into lamina propria Attach gingiva to bone Dentoperiosteal From cementum near the cementoenamel junction, into periosteum of the alveolar crest Anchor tooth to bone; protect periodontal ligament Circular Within free marginal and attached gingiva coronal to alveolar crest, encircle each tooth (“purse string) Maintain contour and position of free marginal gingiva Transeptal From interproximal cementum coronal to alveolar crest, course mesially and distally in interdental area into cementum of adjacent tooth Maintain relationships of adjacent teeth; protect interproximal bone
- 70. Secondary Groups Periostogingival From periosteum of the lateral aspect of alveolar process, splay into attached gingiva Attach gingiva to bone Interpapillary Within interdental gingiva (gingival papilla), orofacial course Provide support for interdental gingiva Transgingival Within attached gingiva, intertwining along the dental arch between and around the teeth Secure alignment of teeth in arch Intercircular From cementum on distal surface of a tooth, splaying buccally and lingually around adjacent tooth and inserting on mesial cementum of next tooth Stabilize teeth in arch Intergingival Within attached gingiva, immediately subjacent to epithelial basement membrane, course mesiodistally Provide support and contour of attached gingiva Semicircular From cementum on mesial surface of tooth, course distally, insert on cementum of distal surface of same None intuitively obvious
- 73. The color of attached and marginal gingiva is generally described as “coral pink” Produced by the vascular supply ,the thickness,degree of keratinization of epithelium, the presence of pigment cells The attached gingiva is demarcated from the adjacent alveolar mucosa on the buccal aspect by a clearly defined mucogingival line DIFFRENCES BEWEEN ALVEOLAR MUCOSA AND ATTACHED GINGIVA ALVEOLAR MUCOSA ATTACHED GINGIVA COLOR Red Pink SURFACE TEXTURE Smooth and shiny Shiny EPTHELIUM Thinner non keratinised .Rete pegs absent Thicker parakeratinised .Rete pegs present CONNECTIVE ISSUE More loosely arranged.More blood vessels Not so loosely arranged.Moderate blood vessels
- 74. The gingiva is considered the most frequently pigmented tissue in the oral cavity Gingival pigmentation may be classified as Physiologic or Pathologic Physiologic gingival pigmentation All patients except albinos have some degree of physiologic melanin distribution throughout epidermis Eumelanin is present in large amounts in individuals with dark skin and hair . Pathologic gingival pigmentation a) Endocrine diseases:Addison’s disease,Albright syndrome,Acromegaly,Nelson’s syndrome b) Heavy metals:e.g.lead,bismuth,mercury,silver arsenic and gold c) Kaposis sarcoma d) Drug induced: chloroquine,quinine,minocycline,zidovudine,chlorpromazine,ketoconazole,bleomycin,cyclophosphamide e) Post inflammatory pigmentation f) Smoking associated melanosis g) Hemangioma h) Amalgam tatoo i) Graphite tatoo j) Nevocellular nevus and blue nevus k) Oral melanocanthoma l) Mucosal melanoms m) HIV oral melanosis n) Haemchromatosis o) Gingival tatoo
- 75. Graphite tatoo Amalgam tatoo Blue nevus Smoking associated melanosis
- 76. It depends on the shape of the teeth their alignment in the arch Location and size of the area of proximal contact Dimension of facial and lingual gingival embrasures Marginal gingiva:Scalloped outline Attached gingiva:festooned appearance with intermittent prominence corresponding to contour of roots Teeth placed labially-the normal arcuate contour is accentuated and the gingiva located further apically lingually-gingiva is horizontal and thickened
- 77. Shape of intergingival papilla governed by Contour of the proximal tooth surfaces Location of gingival embrassure Shape of gingival embrassure Narrow inter dental gingiva Broad interdental gingiva Proximal surface Flat Flare Roots Close together Wide Interdental bone Thin mesiodistally Broad
- 78. Firm and resilient The collagenous nature of the lamina propria and its continuity with the mucoperiosteum of the alveolar bone determine the firmness of the attached gingiva The gingival fibres contribute to the firmness of the gingival margin
- 79. Textured surface similar to an orange peel referred as stippled It is best viewed by drying the gingiva Attached gingiva is stippled ;marginal gingiva not The central portion of the interdental papillae is usually stippled,but the marginal borders are smooth Stippling is produced by alternate rounded protuberances and depressions in the gingival surface Stippling is a form of adaptive specialization or reinforcement of function
- 80. Refers to the level at which the gingival margin is attached to the tooth Tooth erupts into the oral cavity the margin and sulcus are at the tip of crown; as eruption progresses they are seen closer to the root Active eruption-movement of teeth in the direction of occlusal plane Passive eruption-exposure of the tooth by apical migration of gingiva Gottlieb and Orban: active and passive eruption go hand in hand Active eruption is coordinated with attrition;the teeth erupt to compensate for tooth substance worn away by attrition Attrition reduces the clinical crown and prevents it from becoming dispropotionately long in relation to the clinical root, thus avoiding excessive leverage on periodontal tissue Rate of active eruption keeps pace with tooth wear in order to preserve vertical dimension Exposure of teeth via the apical migration of the gingiva is called gingival recession or atrophy
- 82. Consists of an intricate web of arteries that originate from the carotid artery Buccal mucosa-tiny divisions of the buccal artery and posterior superior alveolar artery Palate-greater palatine artery, division of the descending palatine artery originating from the maxillary artery Floor of the mouth, mandibular lingual gingiva- sublingual & submental arteries Labial gingiva overlying the mandible –small divisions from the inferior alveolar artery(incisive and mental artery) Labial gingiva overlying maxilla-anterior superior alveolar artery
- 84. The innervation of the oral gingiva is unique because all the nerves supplying the gingival mucosa originate from the mandibular and maxillary branches of the trigeminal nerve Mandible Labial part-buccal branch of mandibular nerve,and incisive branch of mental nerve Lingual part-lingual nerve Maxilla Labial part –posterior,middle,and anterior –superior alveolar nerve Palatal part-greater palatine and nasopalatine
- 87. AREA LYMPH NODE Mandibular incisor area Submental lymph nodes Maxillary palatal gingiva Deep cervical lymphnodes Buccal gingiva of maxilla and buccal &lingual gingiva in mandibular premolar area Submandibular lymphnode
- 89. Clinical periodontology-10,11,12th edition Caranza Clinical periodontology and Implant dentistry –Niklaus P.Lang,Jan Lindhe Text book of periodontics –Shalu Bathla A textbook of periodontics and implantology –Nitin Saroch Journal of dentistry –Attached gingiva…Then and Now.Vol:4,Issue:1 Tissues and cells of periodontium Periodontology 2000, Vol. 3, 1993, 9-38 Histochemistry of gingiva :A review article International Journal of Applied Dental Sciences Development Of Periodontium: A Star In The Making!!! International Journal Of Medical Science And Clinical Inventions Volume 2 issue 08 2015 Anatomy,Head and Neck,Oral gingiva-Adam Koller,Amit Sapra Gingival Biotype Assessment in a Healthy Periodontium:Transgingival Probing Method .Journal of Clinical and Diagnostic Research Gingival Crevicular fluid: An overview.Journal of Pharmacy & Bioallied Sciences Gingival pigmentation(Cause,treatment and histological preview) Future dental journal vol 3,2017