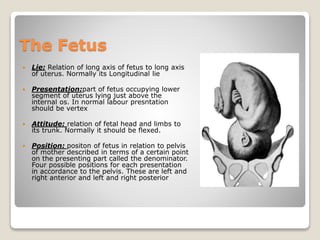
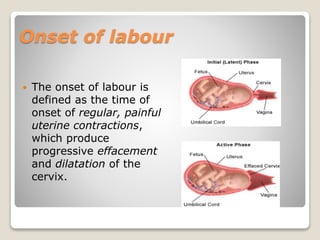
The document provides an overview of normal labour, including definitions, criteria, components, anatomy, onset, stages, monitoring and management. It defines labour and normal labour. The criteria for normal labour includes spontaneous expulsion of a single, full-term fetus presented by vertex within 3-18 hours without complications. The components are the passage (birth canal), passenger (fetus), and power (uterine contractions and abdominal muscles). It describes the anatomy of the female pelvis and fetal skull, as well as the onset, three stages and mechanism of labour. Intrapartum monitoring includes monitoring the mother's temperature, pulse, blood pressure and urine as well as fetal monitoring. Management includes pain relief, hydration, fetal monitoring and managing