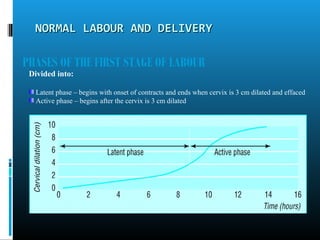
Normal labour is defined as the spontaneous expulsion of a single, mature fetus through the birth canal within 18 hours without complications. It involves 3 stages: 1) cervical dilation, 2) delivery of the baby, 3) delivery of the placenta. The document discusses evaluating and monitoring labour, managing each stage, relieving pain, and recording labour progress on a partogram. Fetal well-being and maternal vital signs are closely watched throughout. [END SUMMARY]