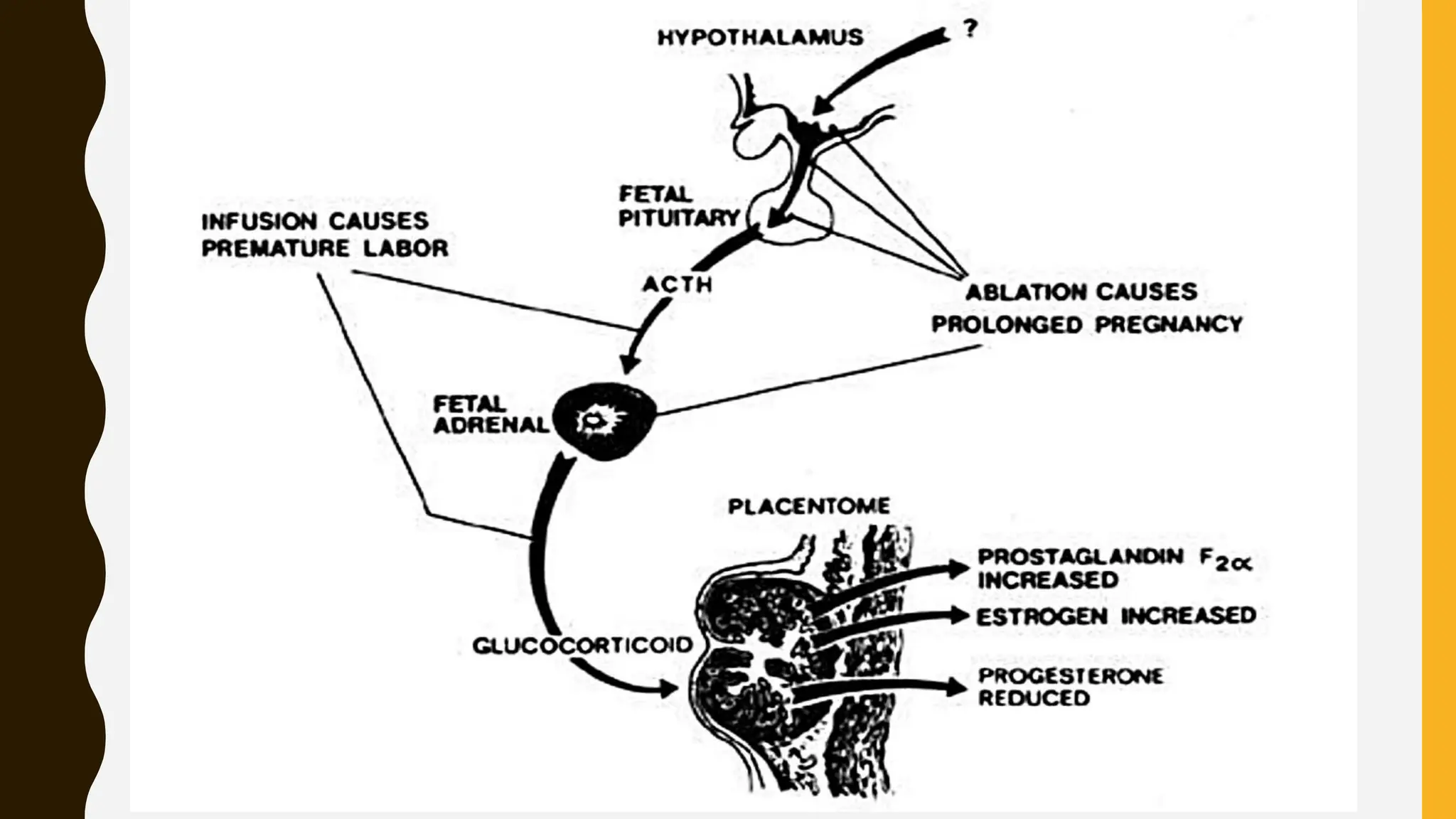
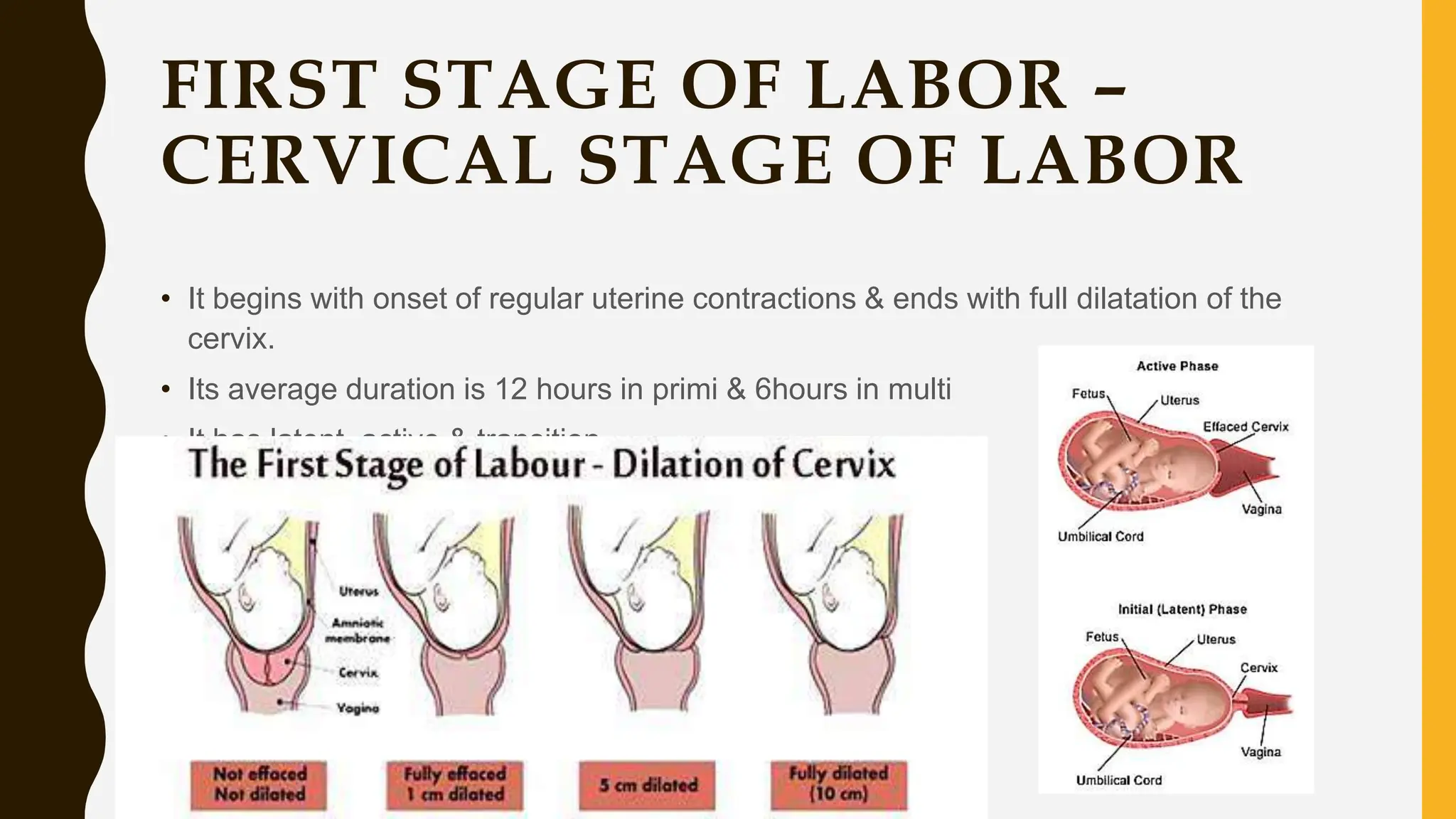
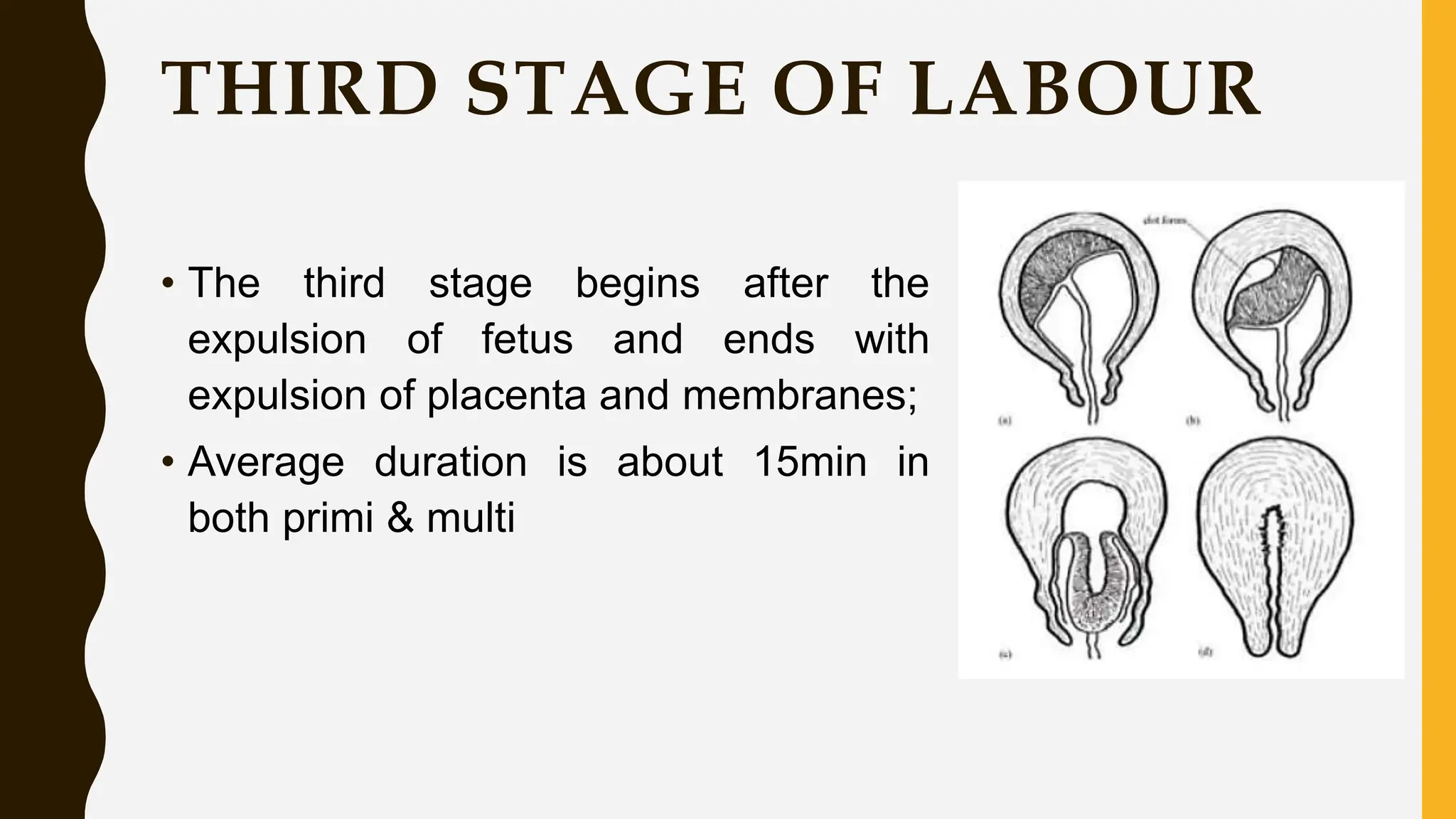
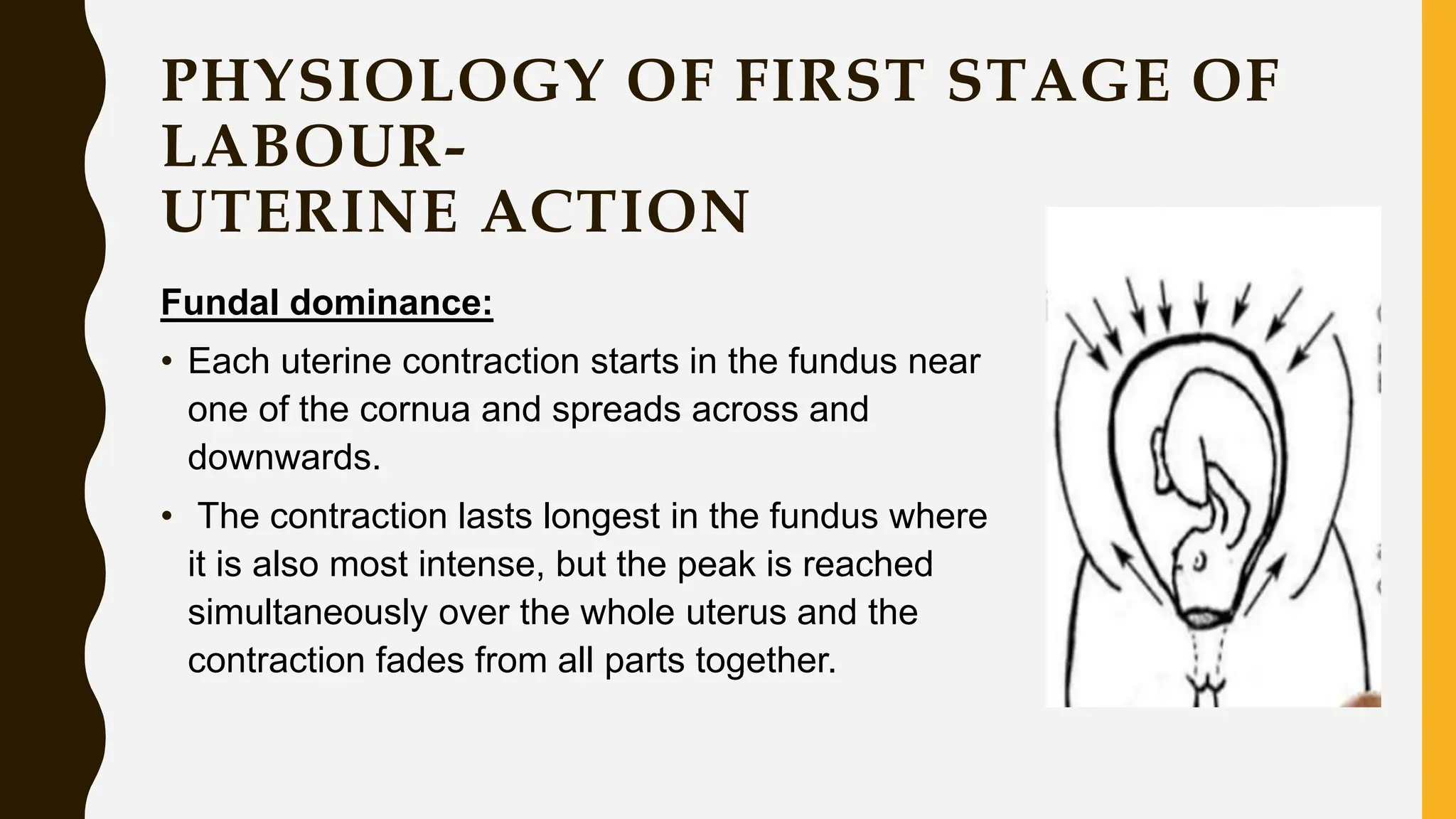
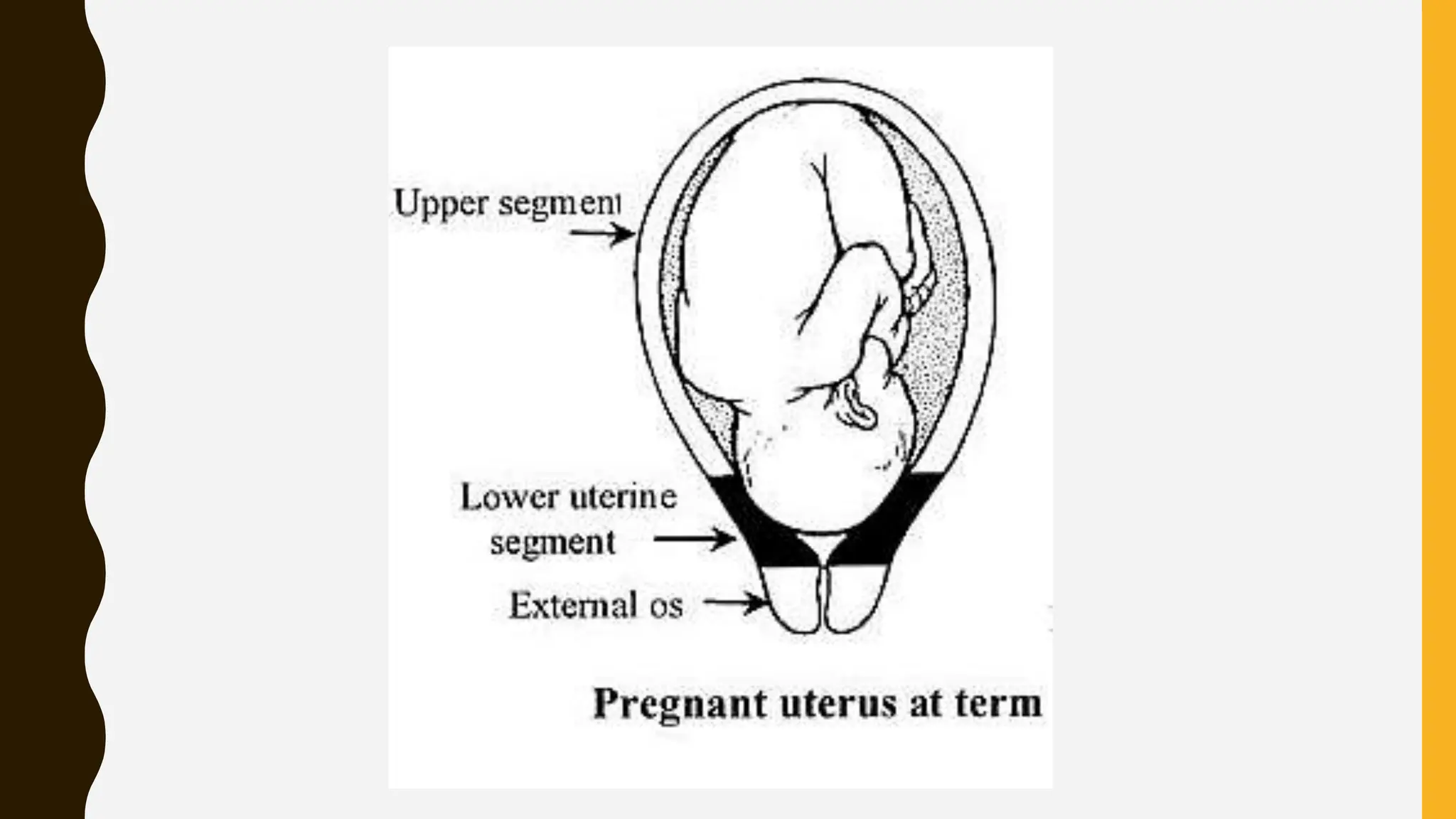
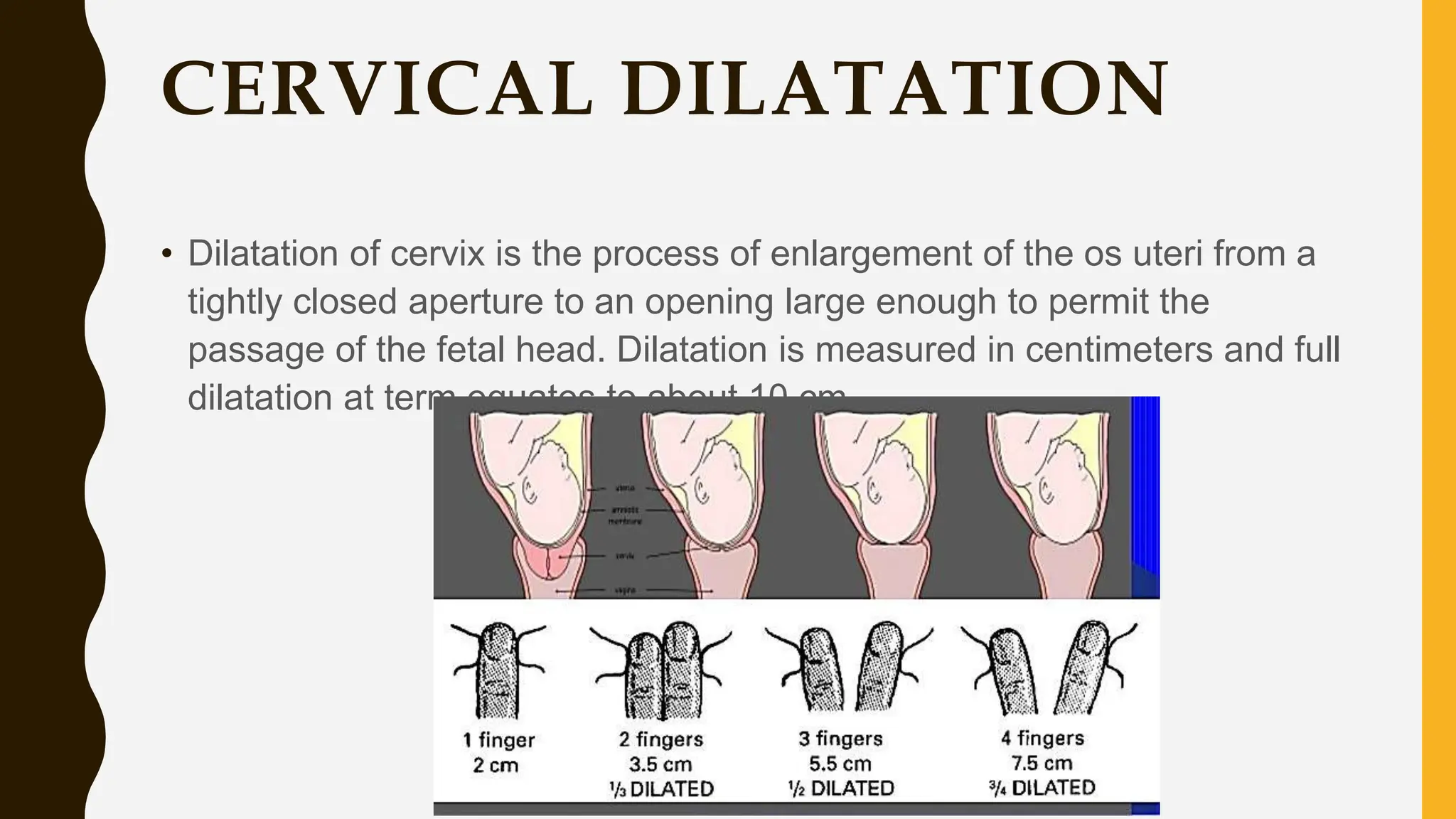
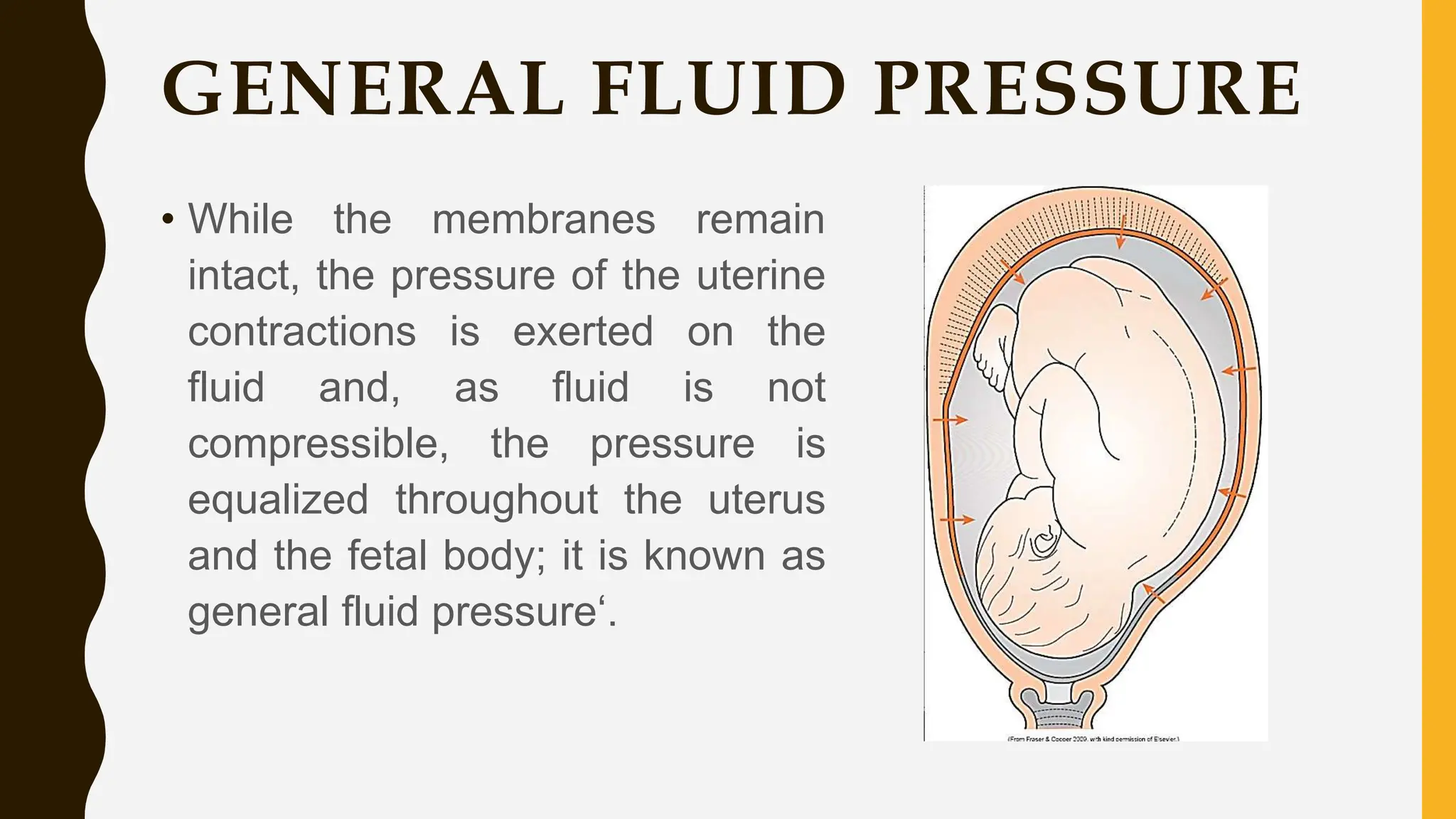
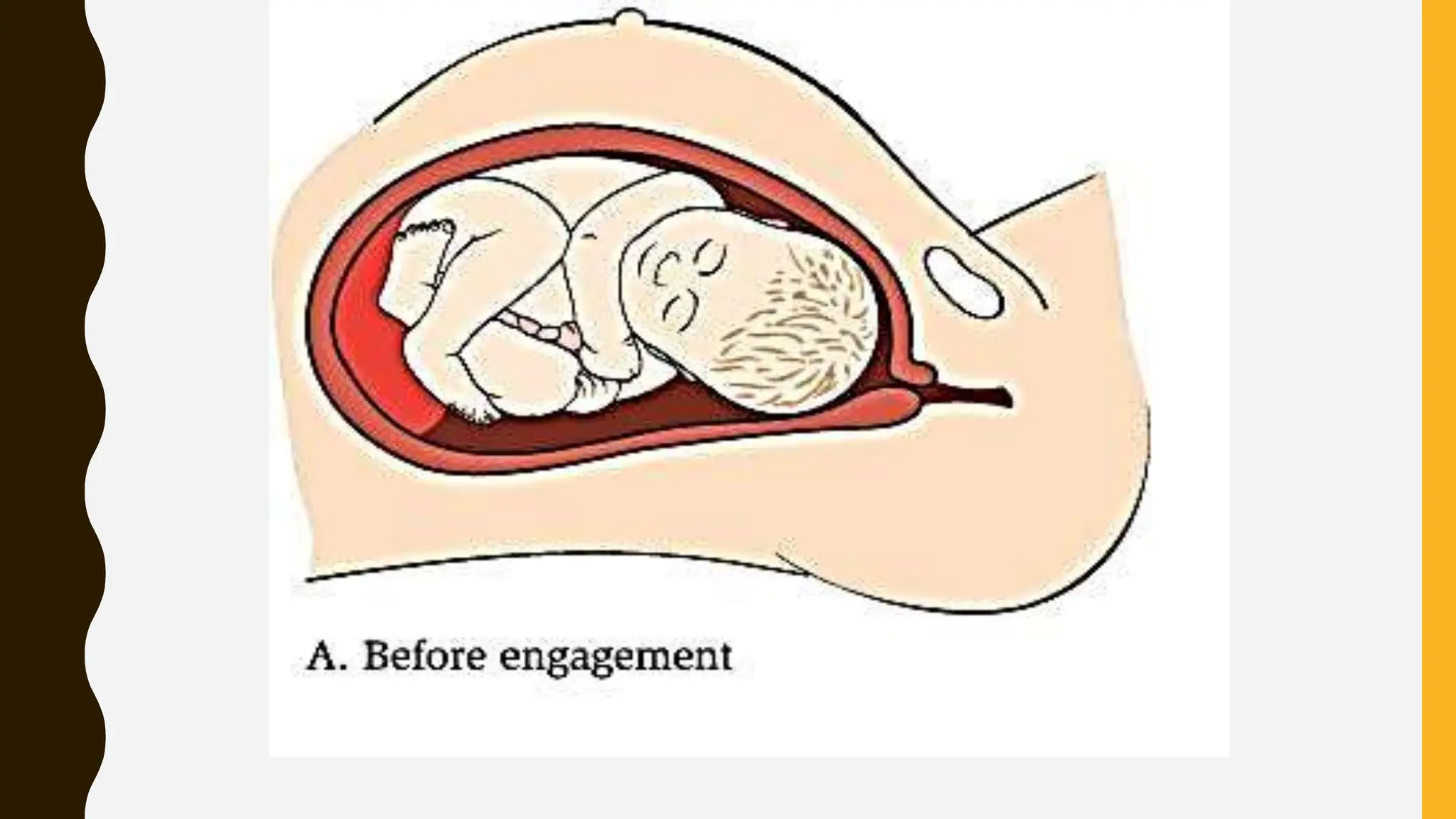
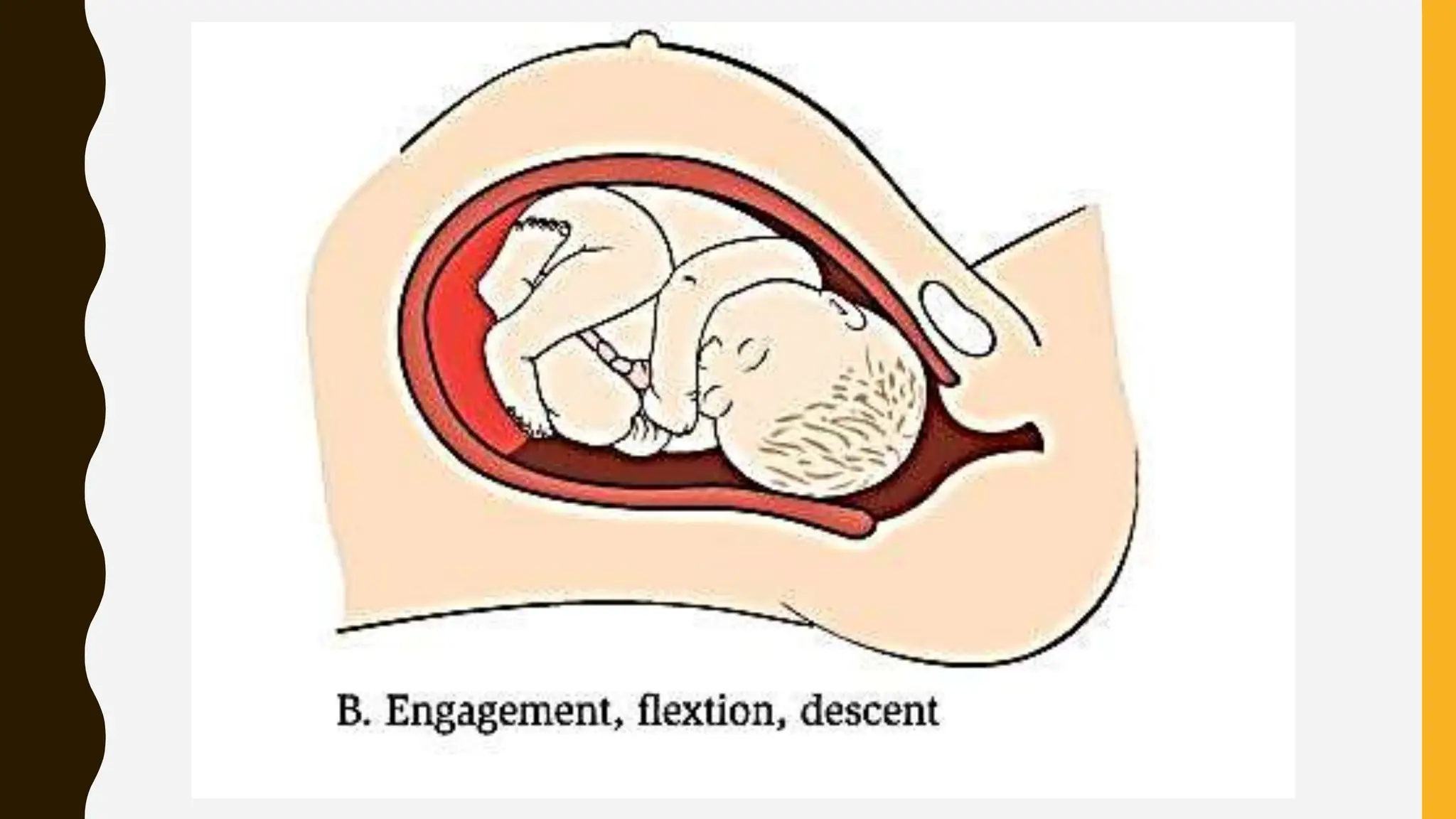
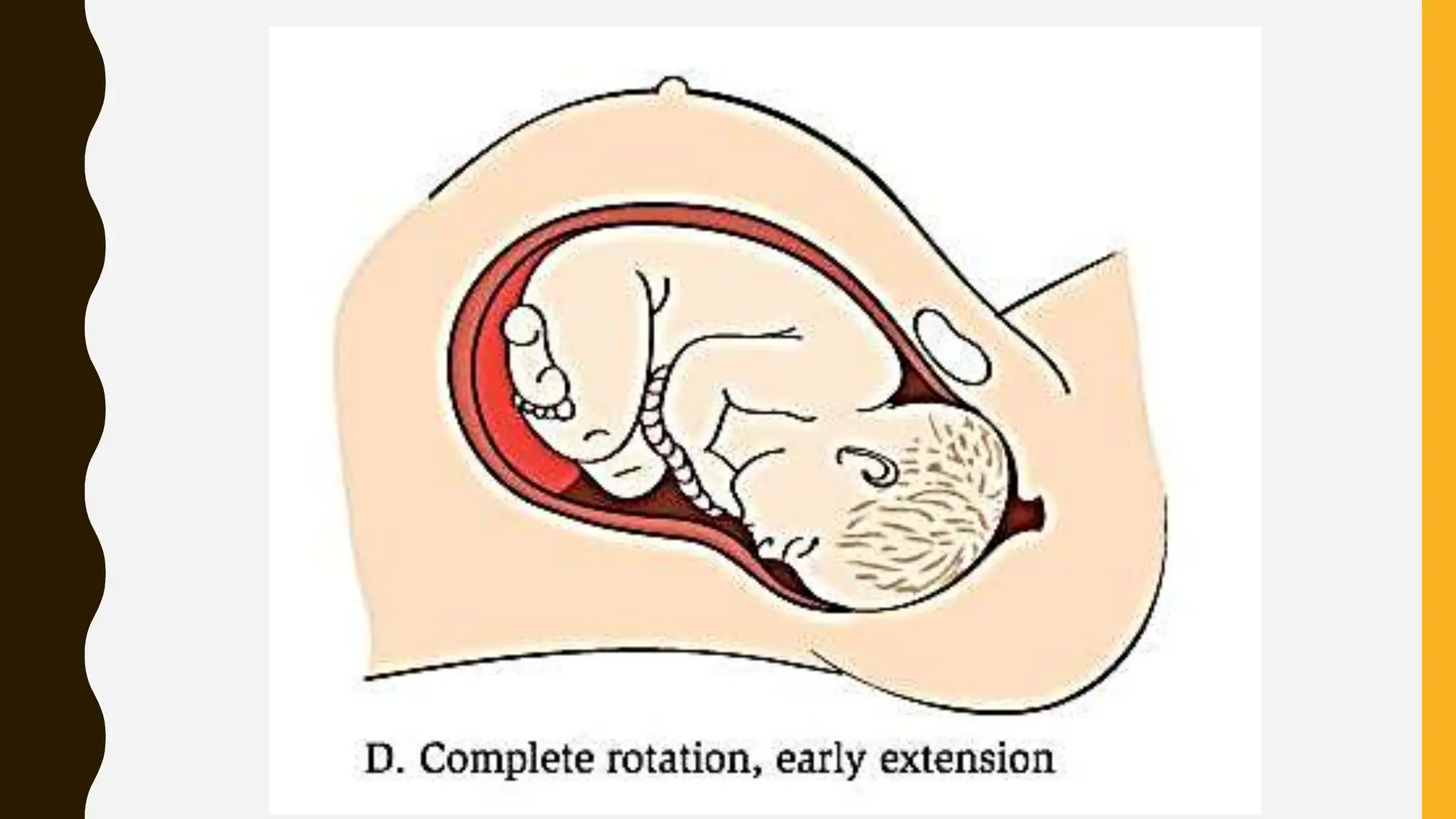
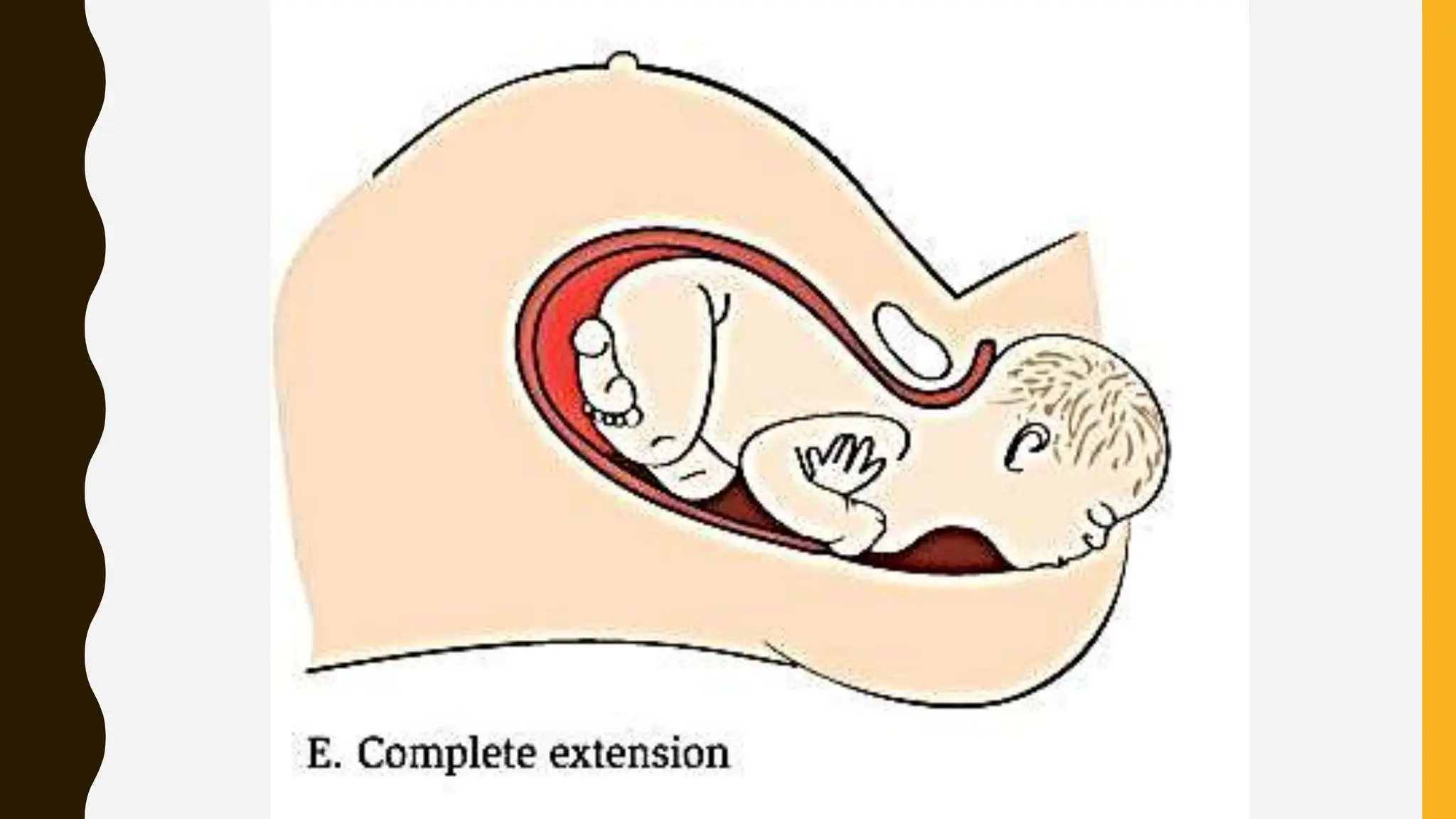
Labor is the process by which uterine contractions result in cervical changes allowing passage of the fetus through the birth canal. It has three stages: first stage involves cervical effacement and dilation; second stage is birth of the fetus; third stage is placental delivery. Uterine contractions are regulated by hormones like progesterone and oxytocin. Contractions start in the fundus and spread across the uterus. The upper segment contracts and retracts while the lower segment dilates, aided by fetal pressing, to progress labor. Average first stage duration is 12 hours in primiparous and 6 hours in multiparous women.