This document provides an overview of normal labor, including:
1. It defines labor and the three stages of labor, and discusses mechanisms and signs of labor onset.
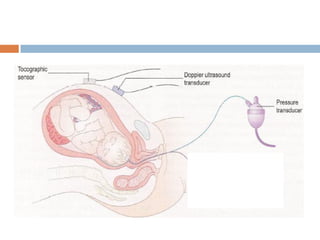
2. Intrapartum monitoring of both mother and fetus is described, including vital signs, fetal heart rate monitoring, and use of the partogram.
3. Management of the three stages of labor is outlined, including pain relief, monitoring, second stage delivery techniques, and third stage placental delivery.