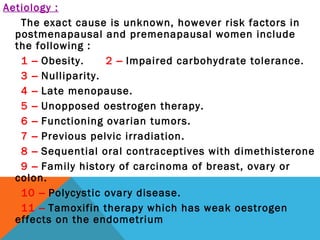
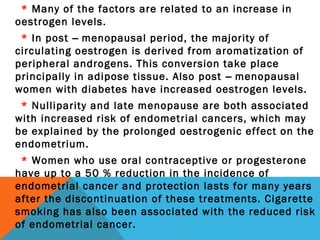
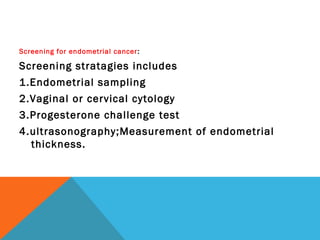
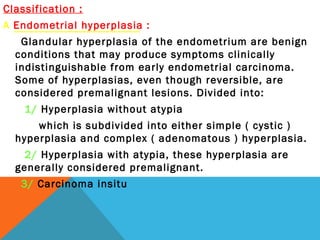
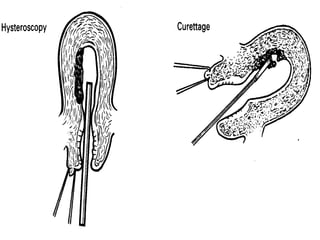
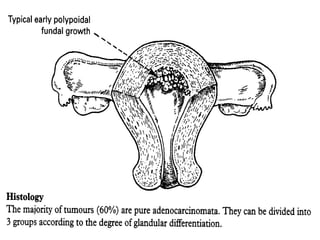
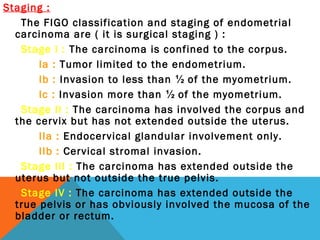
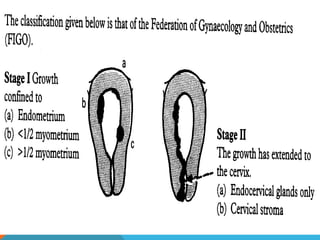
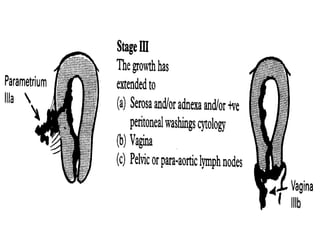
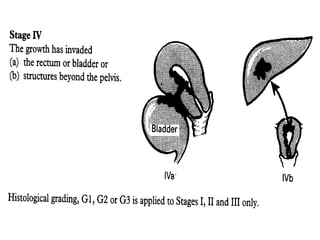
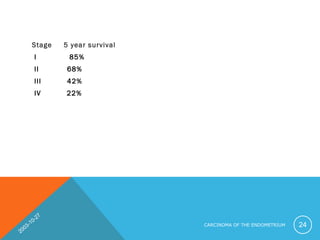
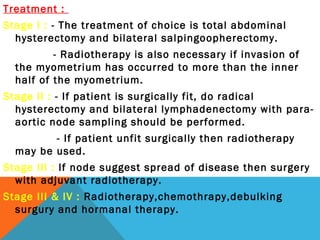
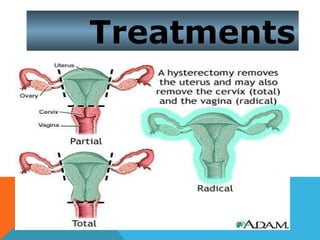
The document discusses malignant disorders of the uterine corpus, specifically endometrial carcinoma. It covers the embryology and anatomy of the uterus, risk factors and epidemiology of endometrial carcinoma, screening and classification. Diagnosis involves endometrial sampling and imaging. Staging is done according to FIGO criteria. Prognosis depends on stage, with stage I having a 5-year survival rate of 85%. Treatment options include surgery, radiation therapy, chemotherapy, and hormone therapy depending on the stage. Follow up after treatment monitors for recurrence or complications.