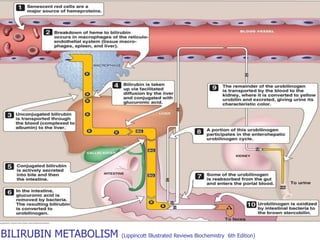
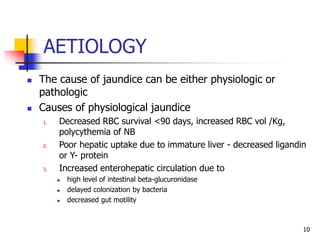
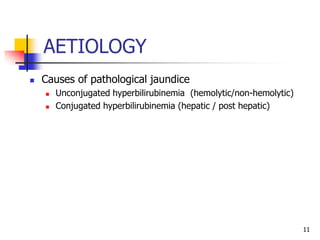
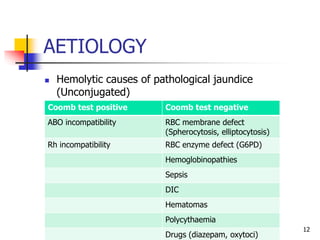
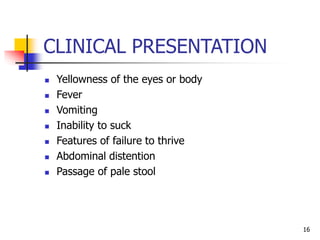
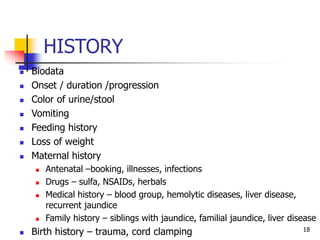
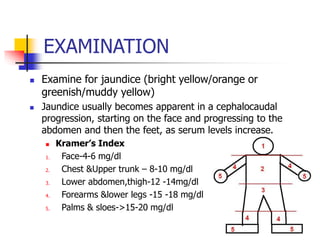
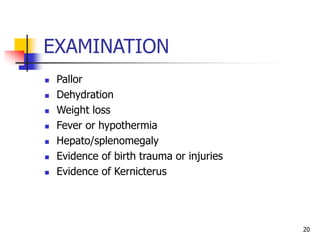
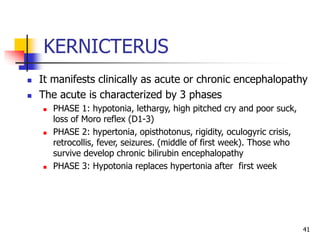
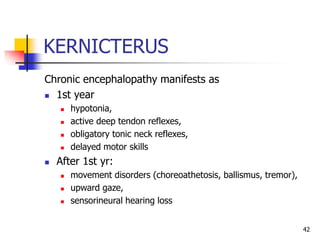
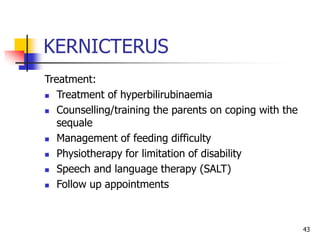
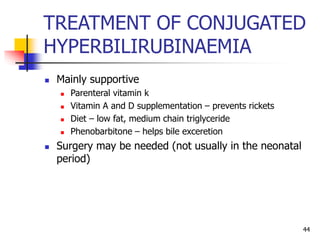
This document provides an overview of neonatal jaundice, including its epidemiology, pathophysiology, etiology, clinical presentation, management, and complications. Key points include:
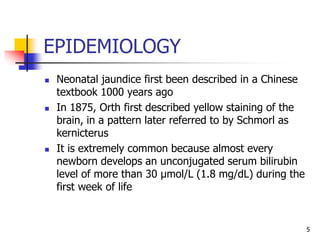
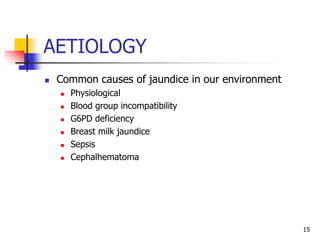
- Neonatal jaundice is common, occurring in 50-80% of newborns, and is usually harmless. It is caused by elevated bilirubin levels in the blood.
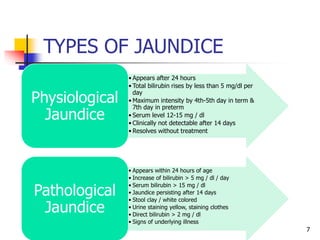
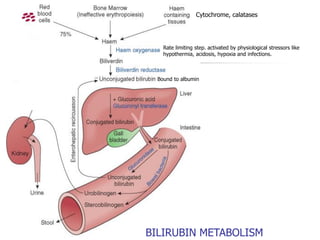
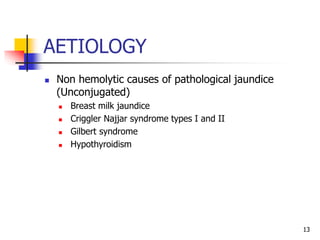
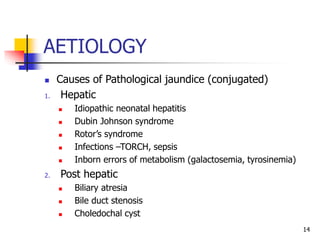
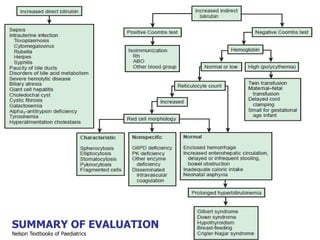
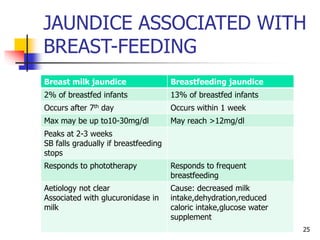
- Jaundice can be physiological or pathological. The causes and management differ depending on whether the elevated bilirubin is conjugated or unconjugated.
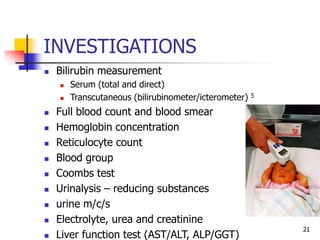
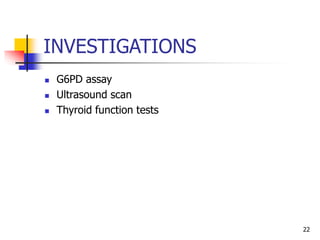
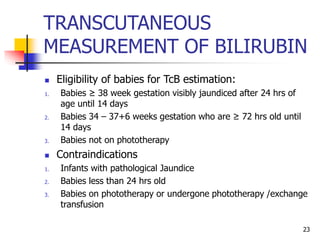
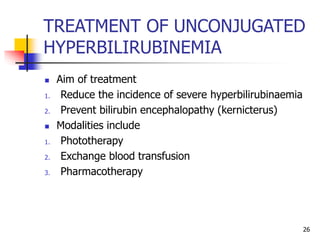
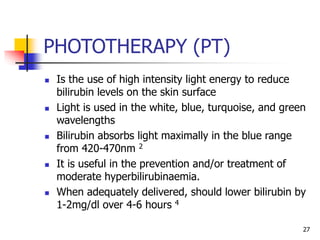
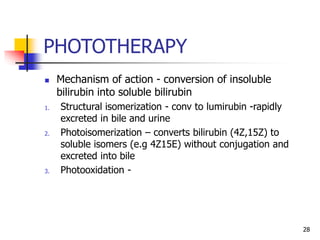
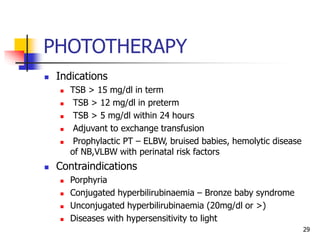
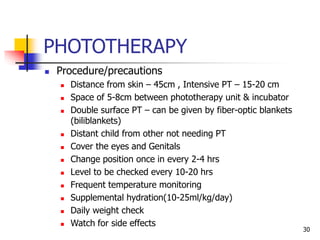
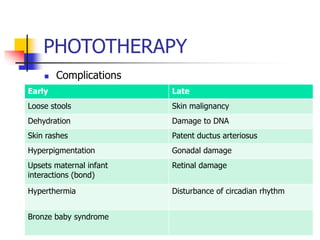
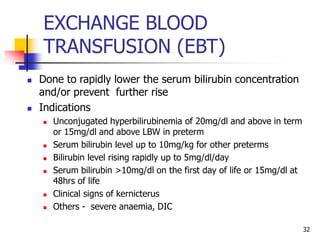
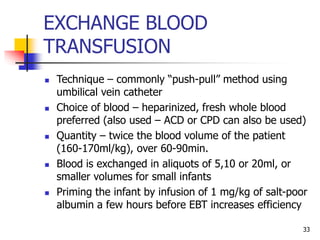
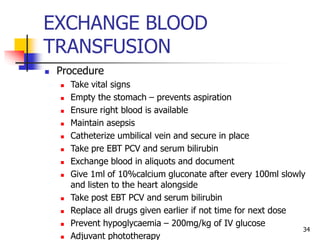
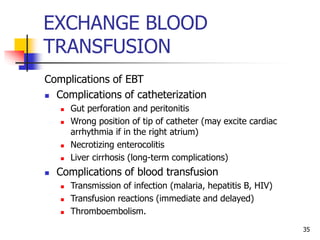
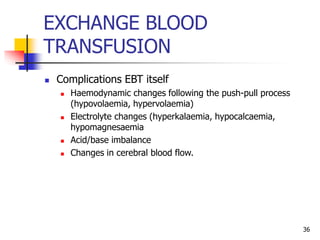
- Evaluation involves clinical exam, bilirubin levels, and other tests to determine the underlying cause. Management includes phototherapy, exchange transfusion, or pharmacotherapy depending on