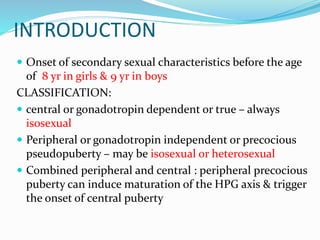
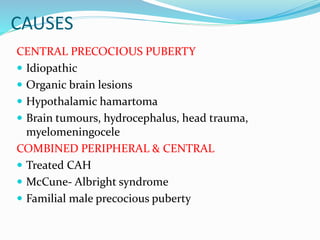
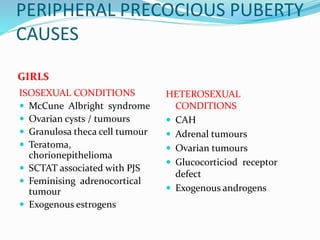
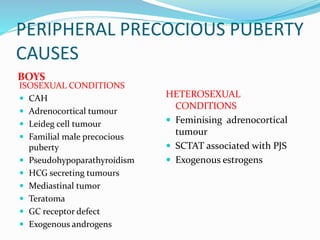
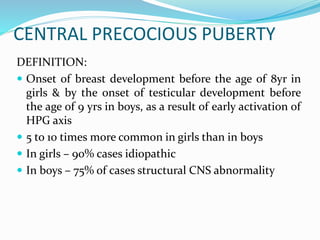
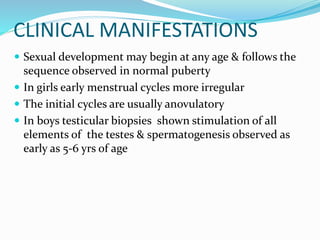
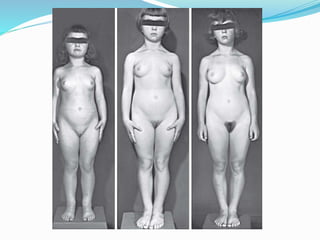
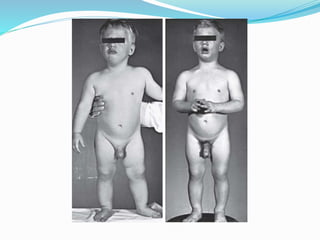
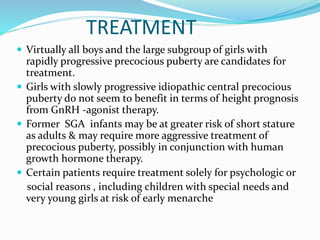
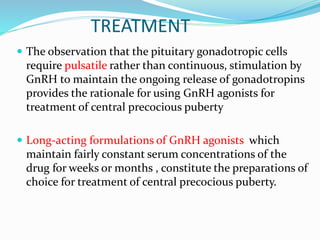
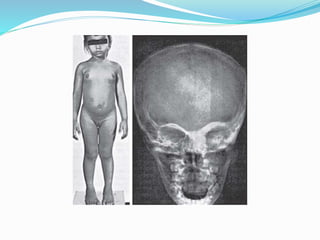
This document discusses precocious puberty, including central precocious puberty and peripheral precocious puberty. Central precocious puberty is the early activation of the hypothalamic-pituitary-gonadal axis, leading to the onset of secondary sexual characteristics before age 8 in girls and 9 in boys. Peripheral precocious puberty is caused by external sex hormones and may be isosexual or heterosexual. McCune-Albright syndrome is a rare cause of peripheral precocious puberty associated with patchy skin pigmentation and fibrous dysplasia. Treatment for central precocious puberty involves suppressing puberty with GnRH agonists to help increase adult height potential.