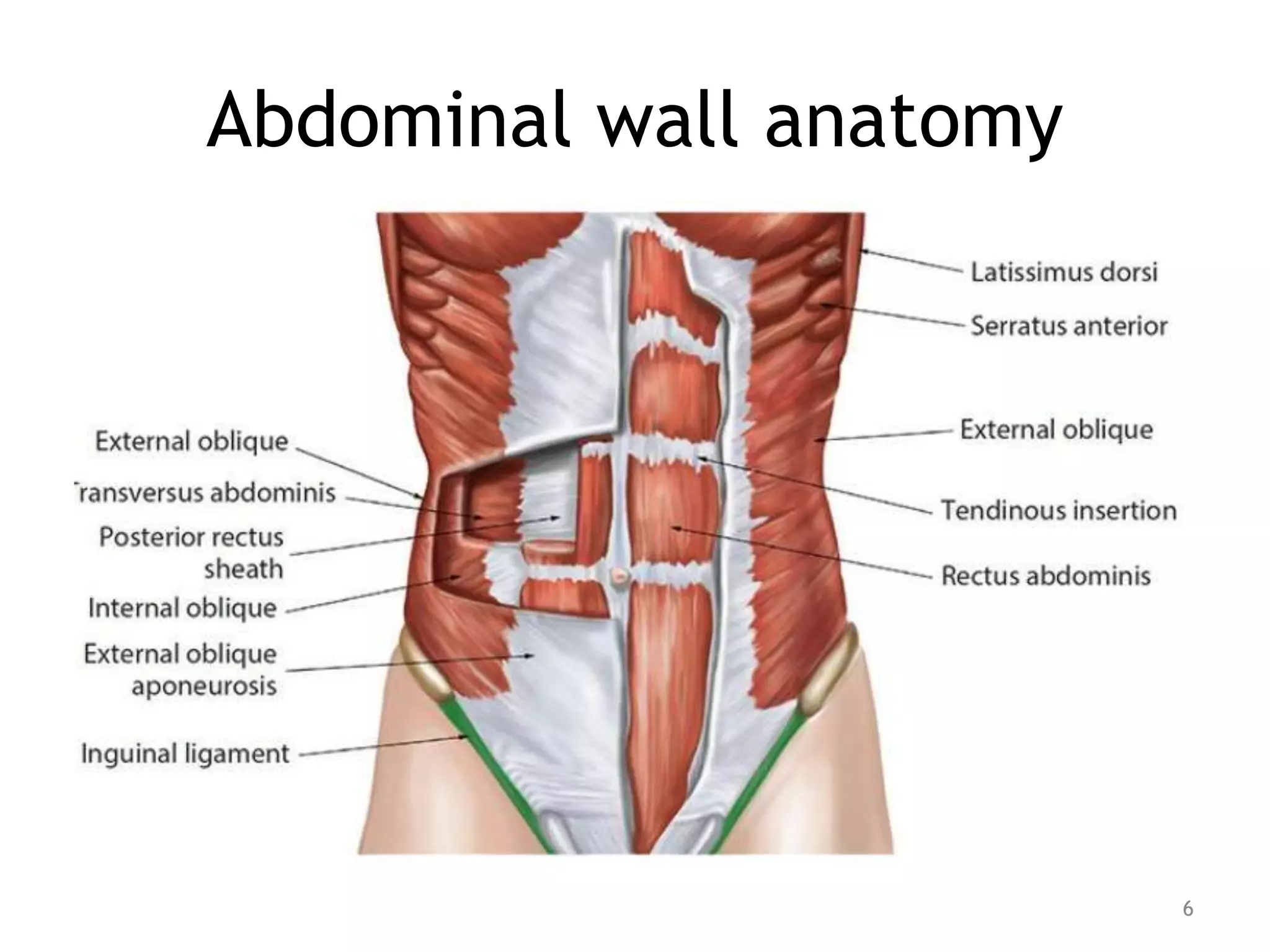
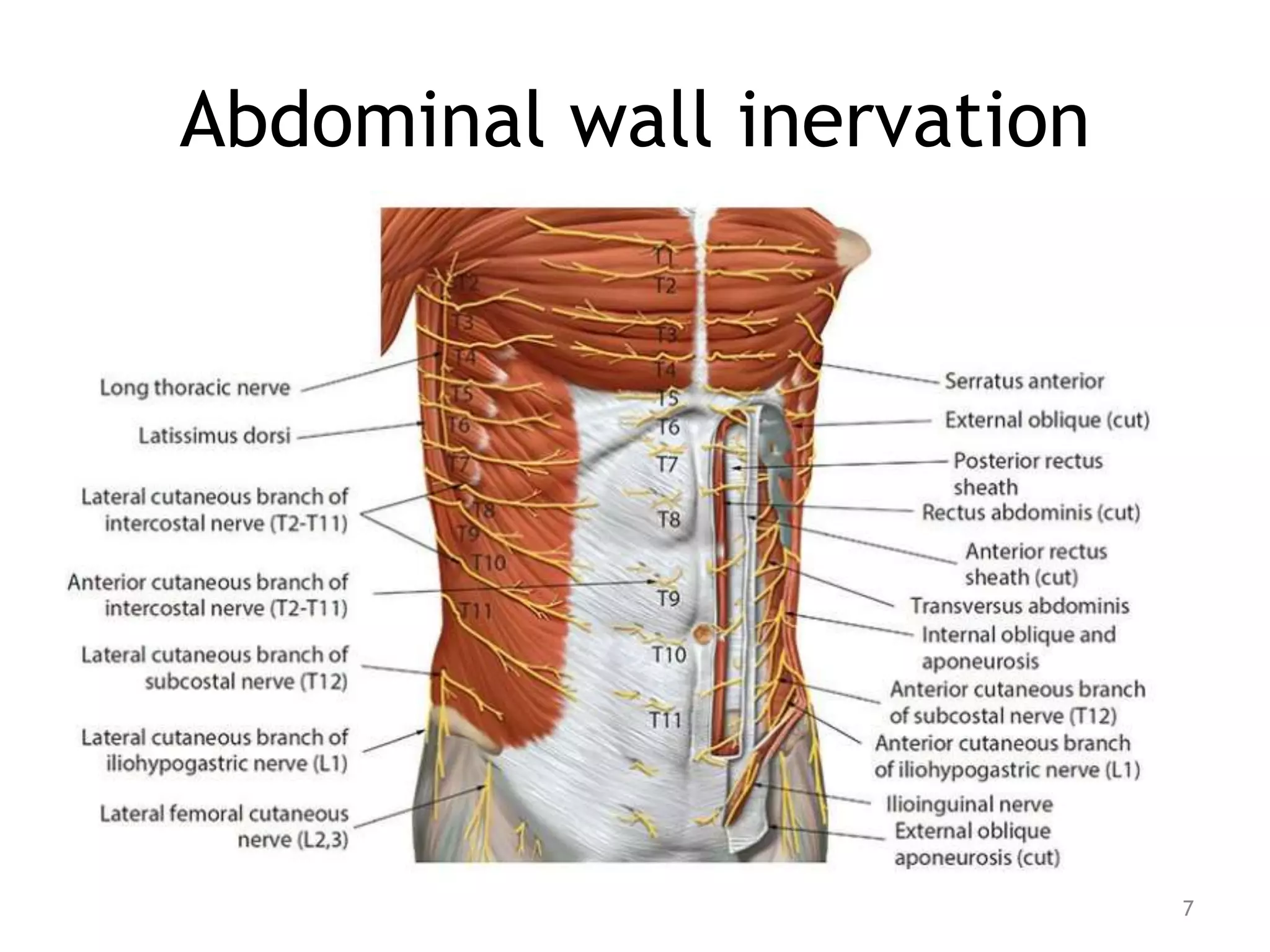
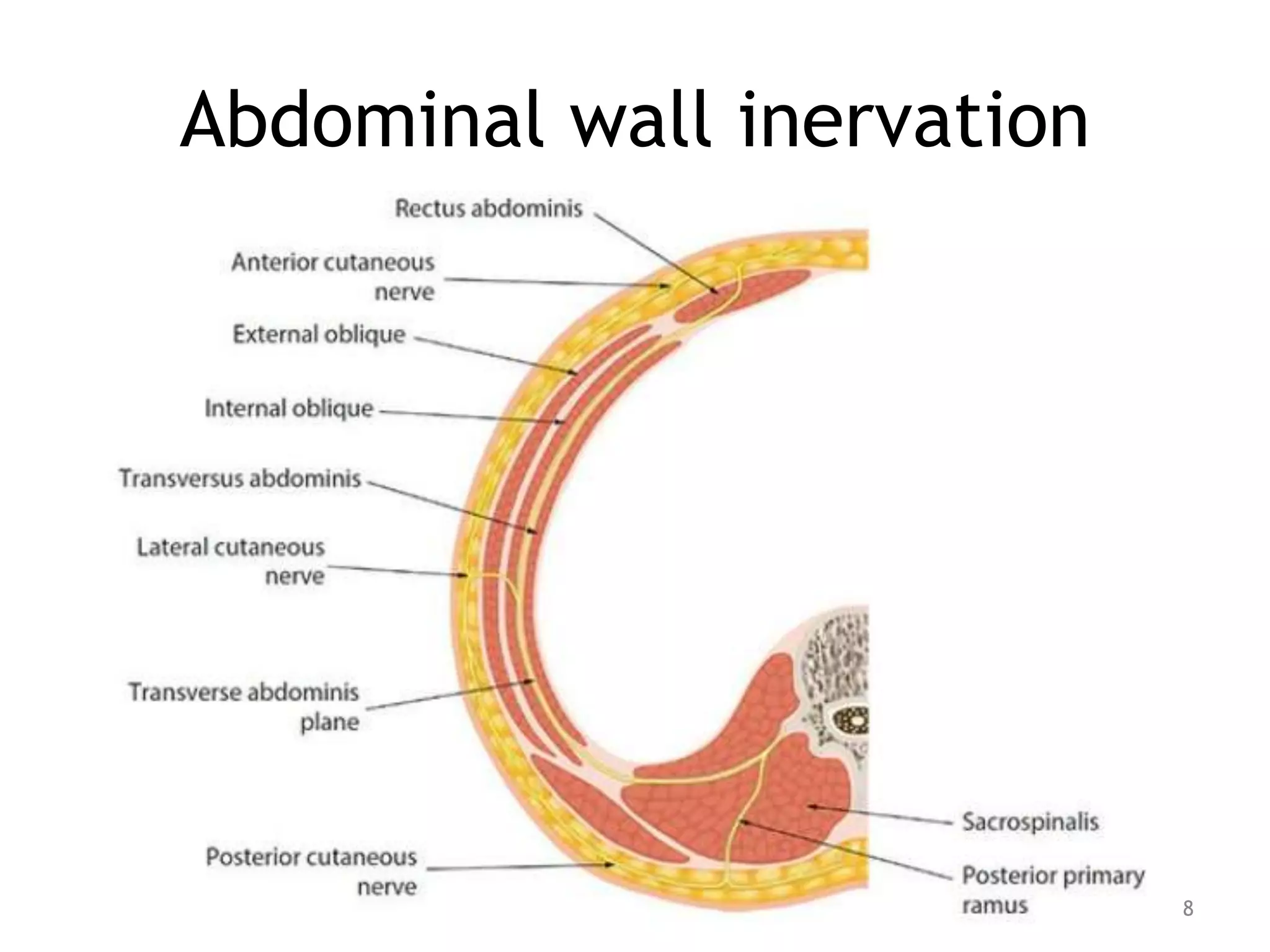
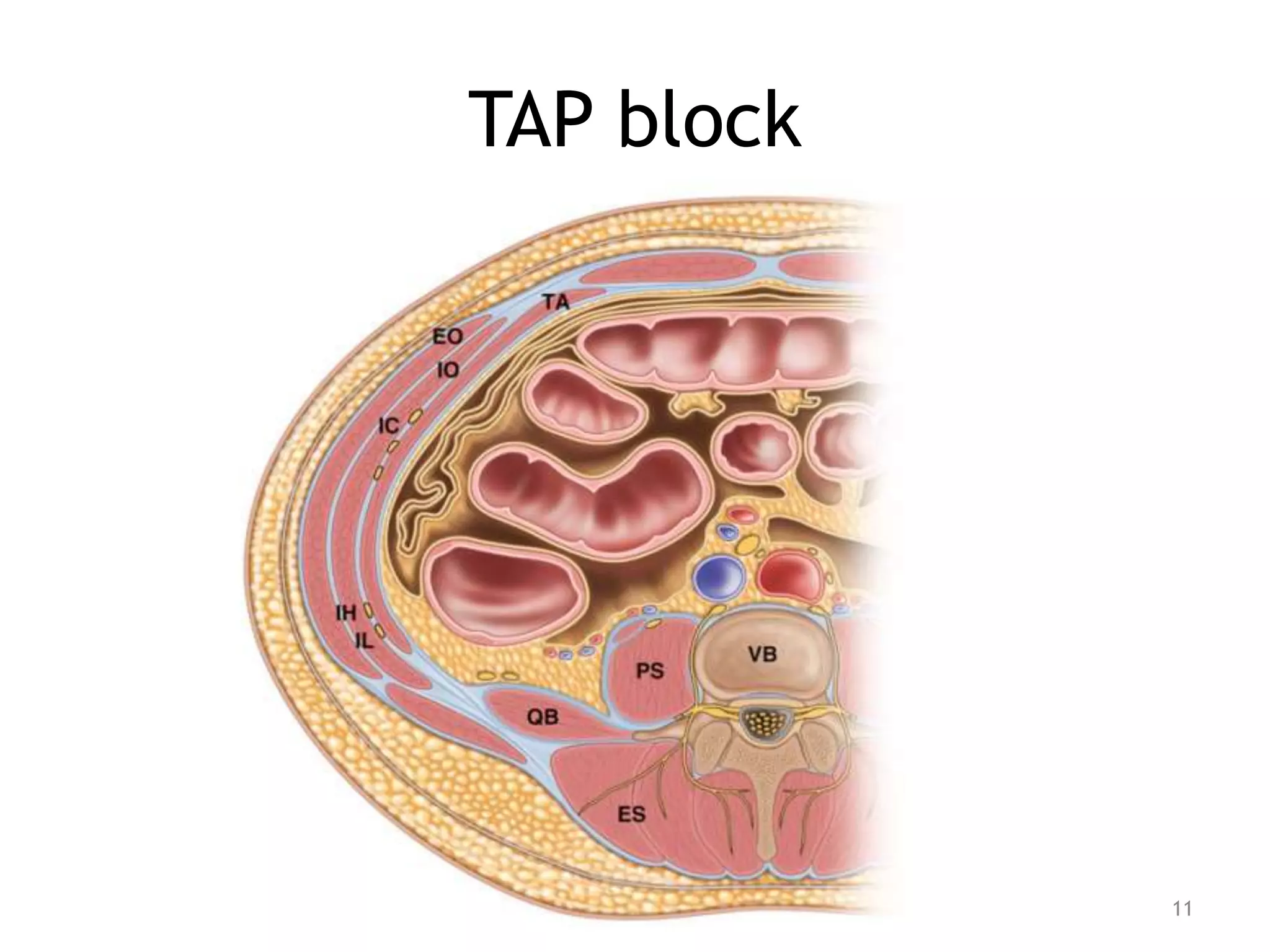
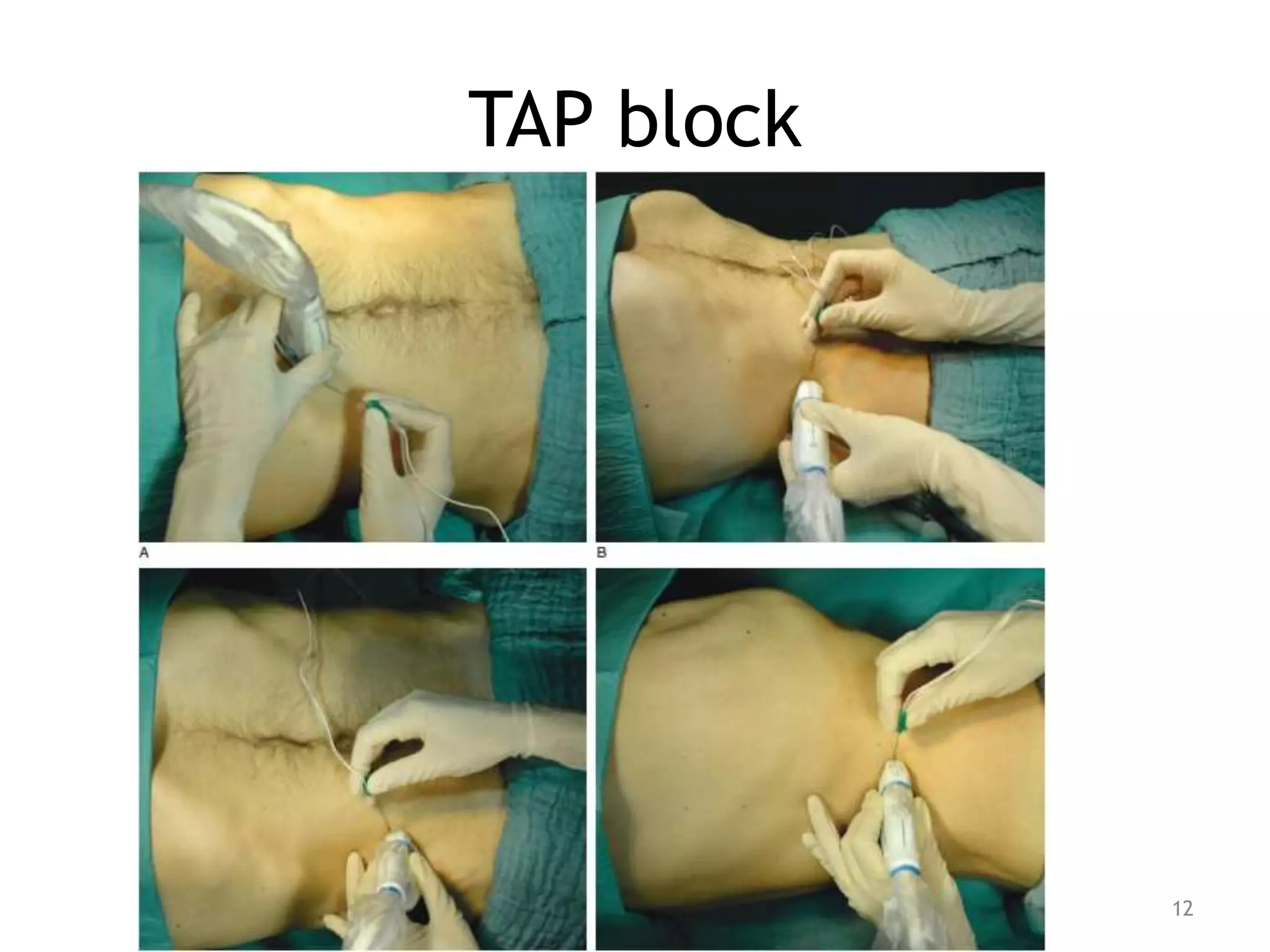
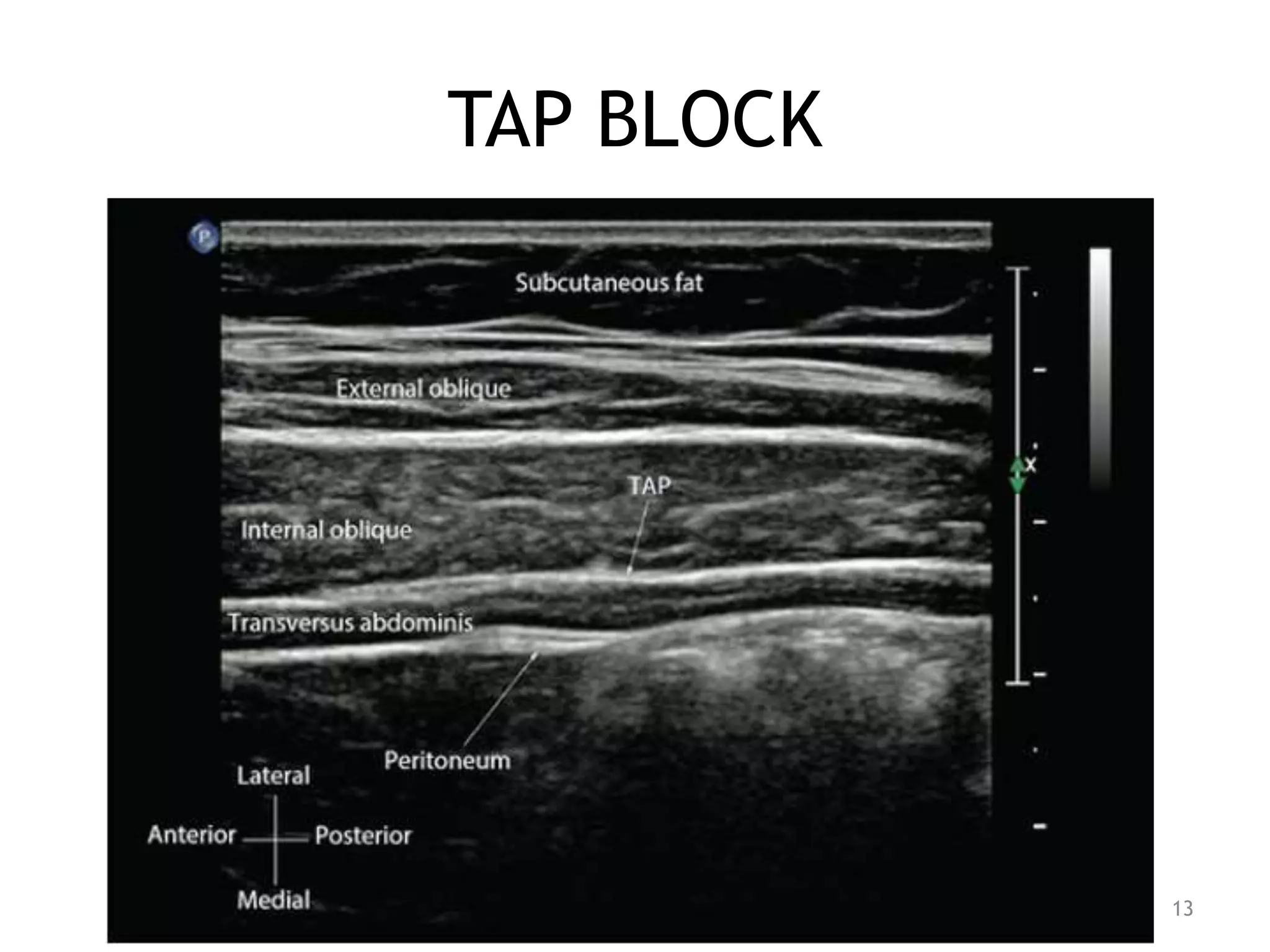
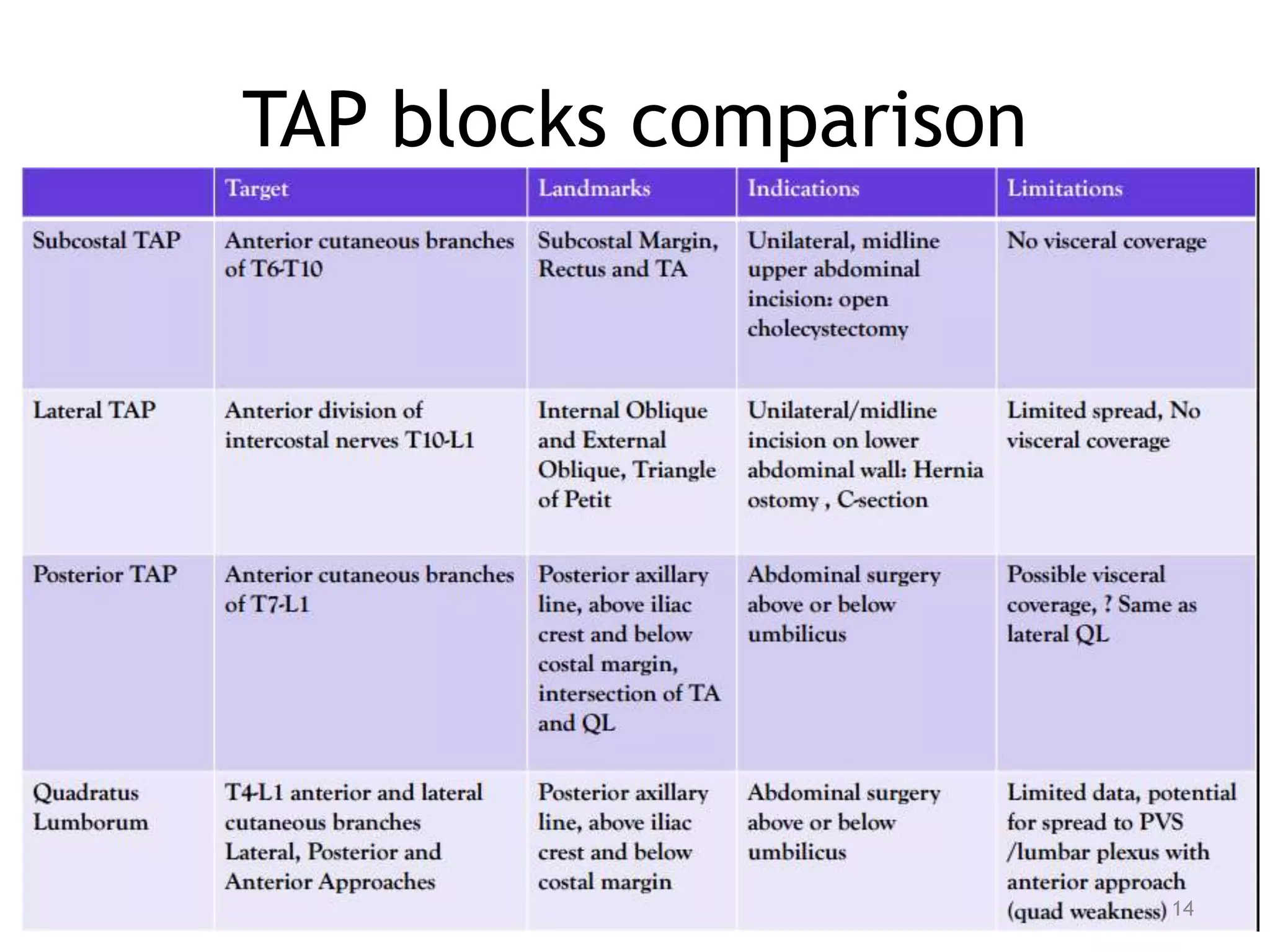
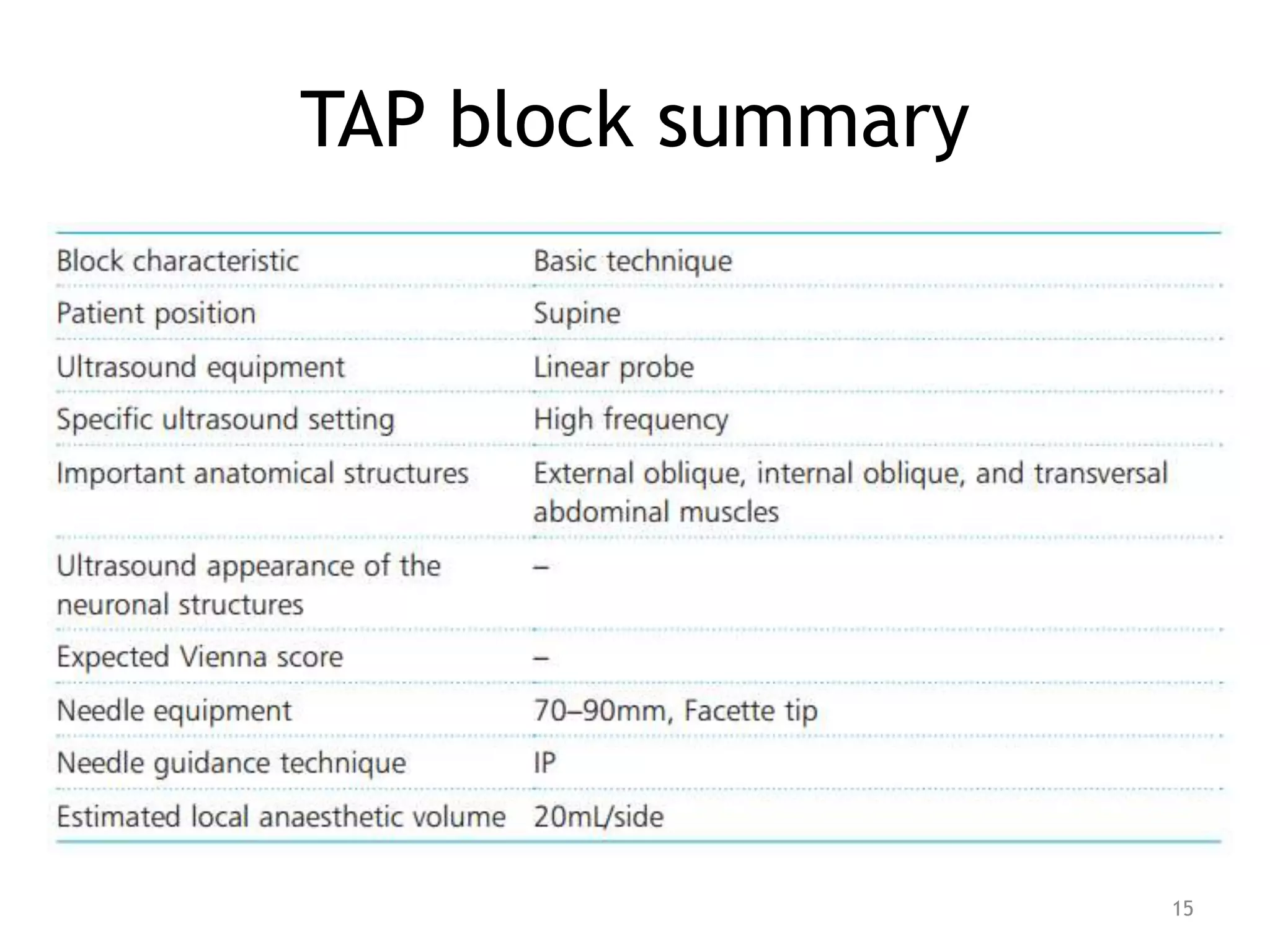
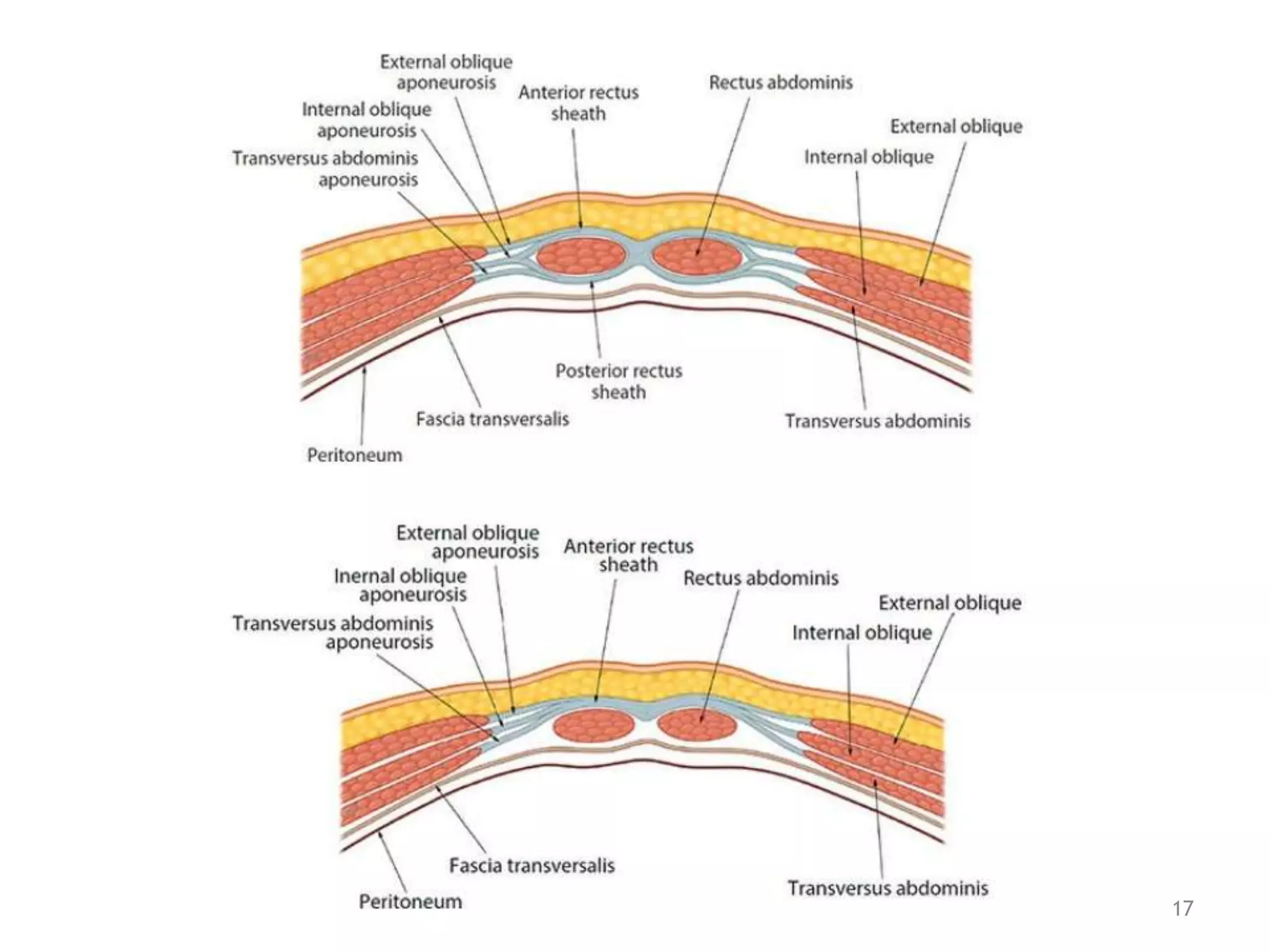
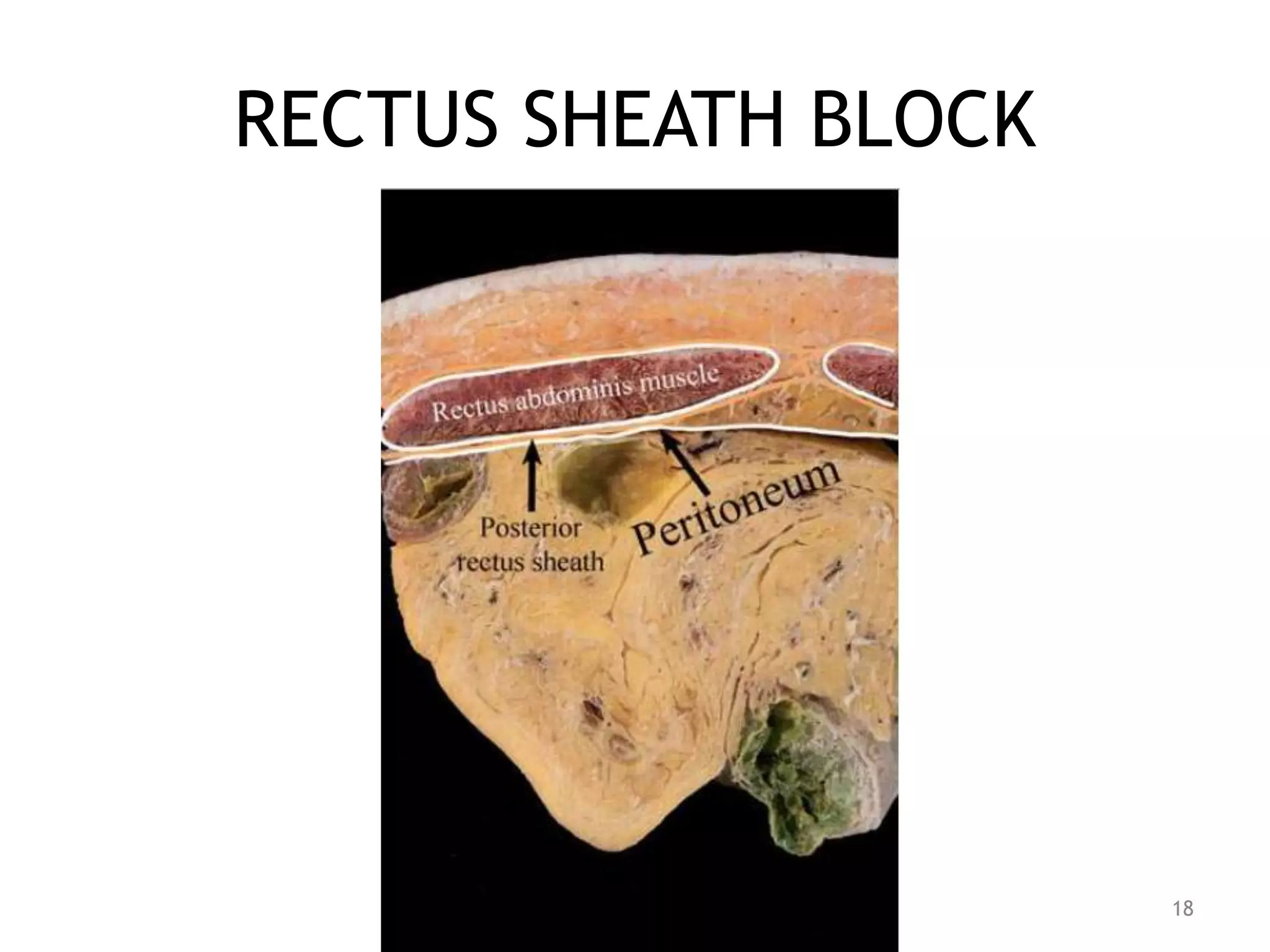
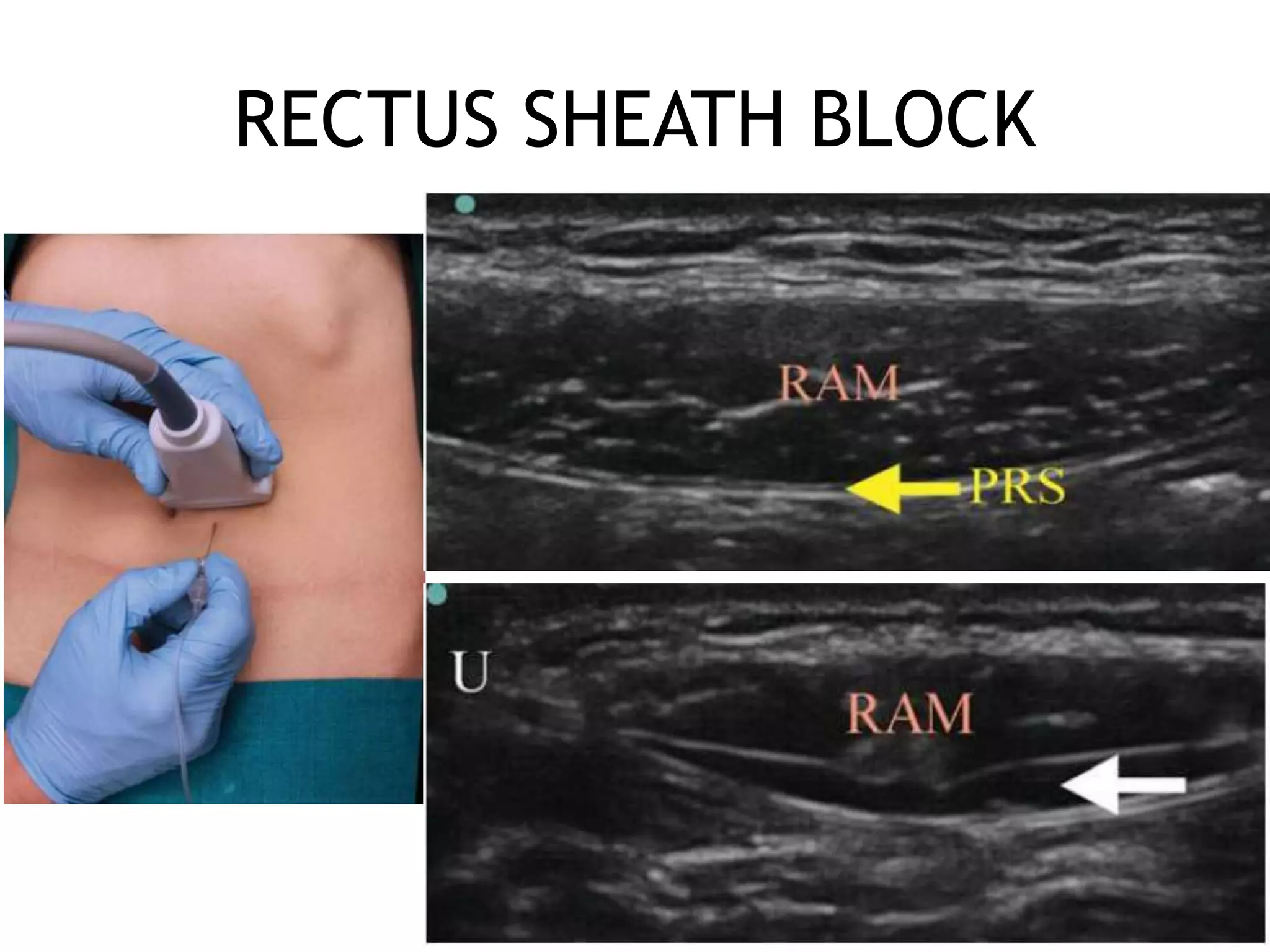
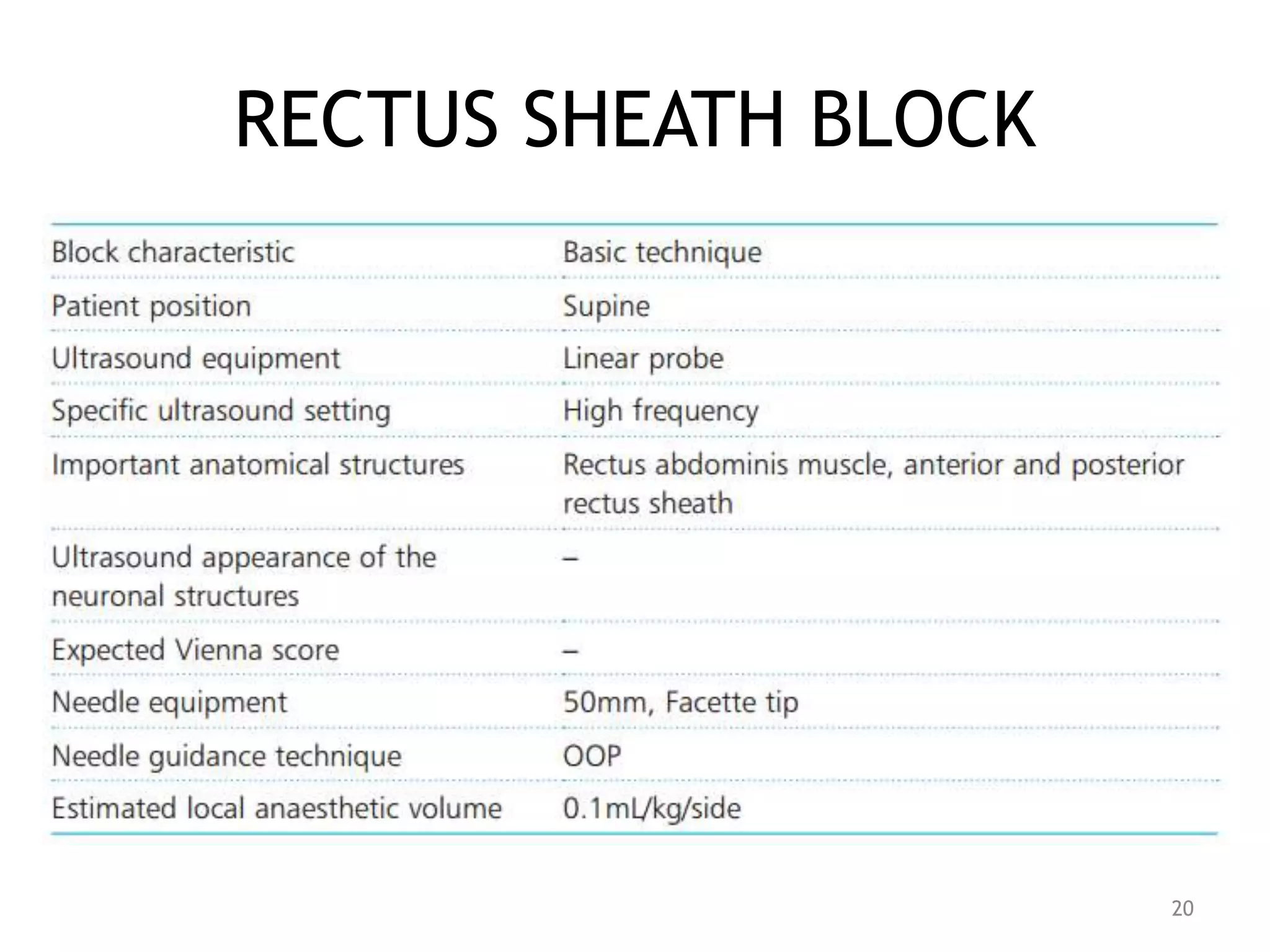
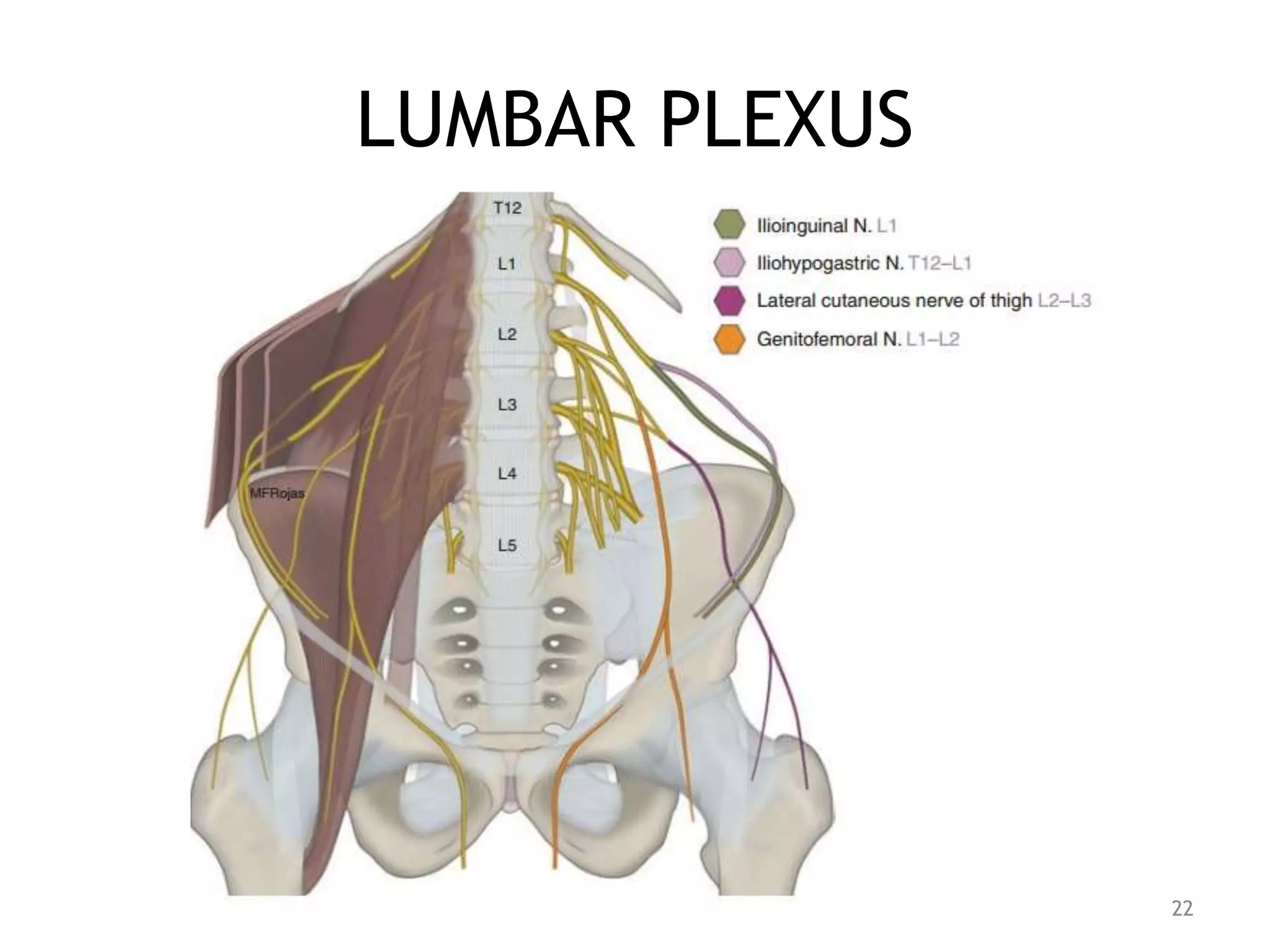
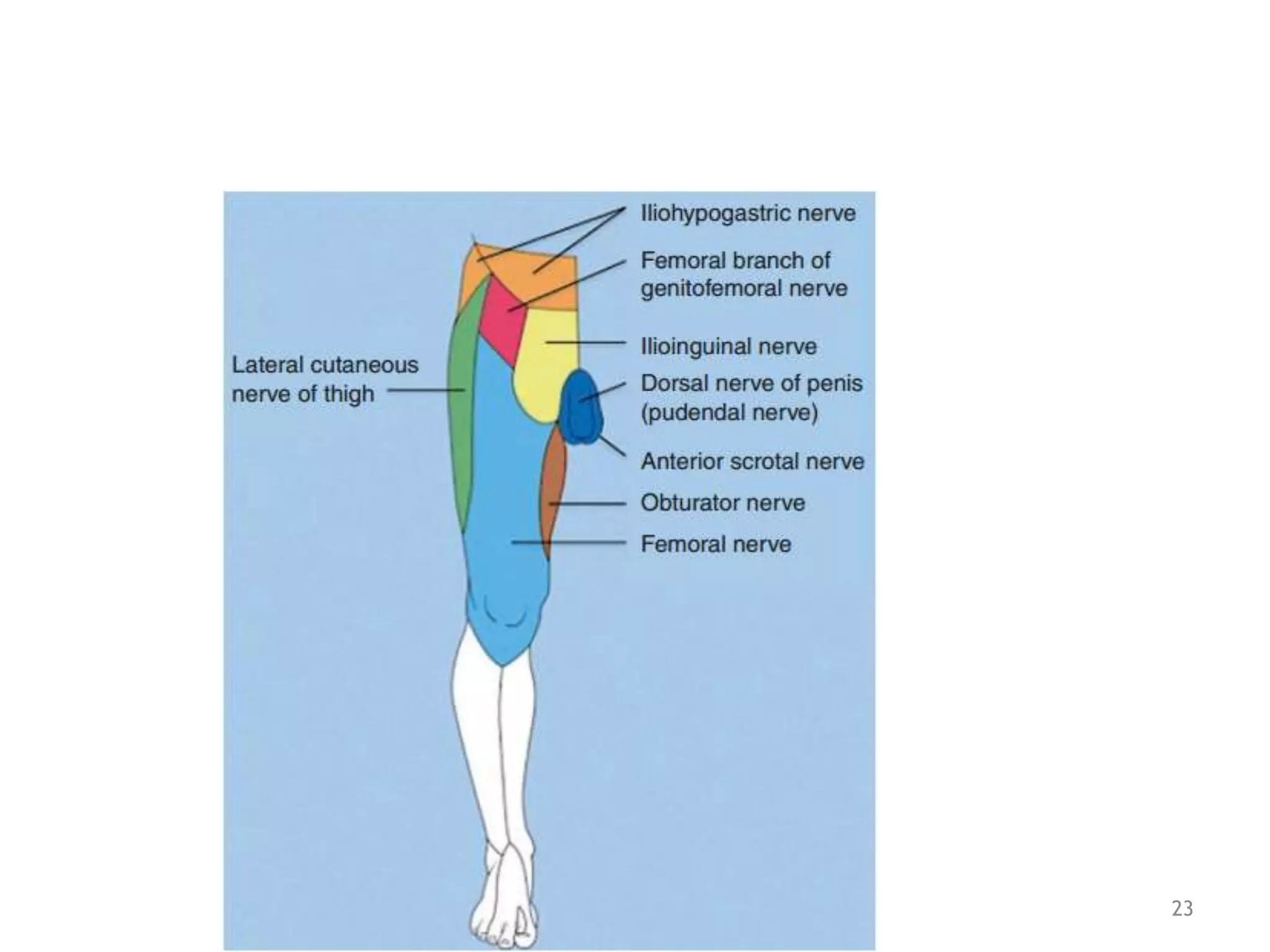
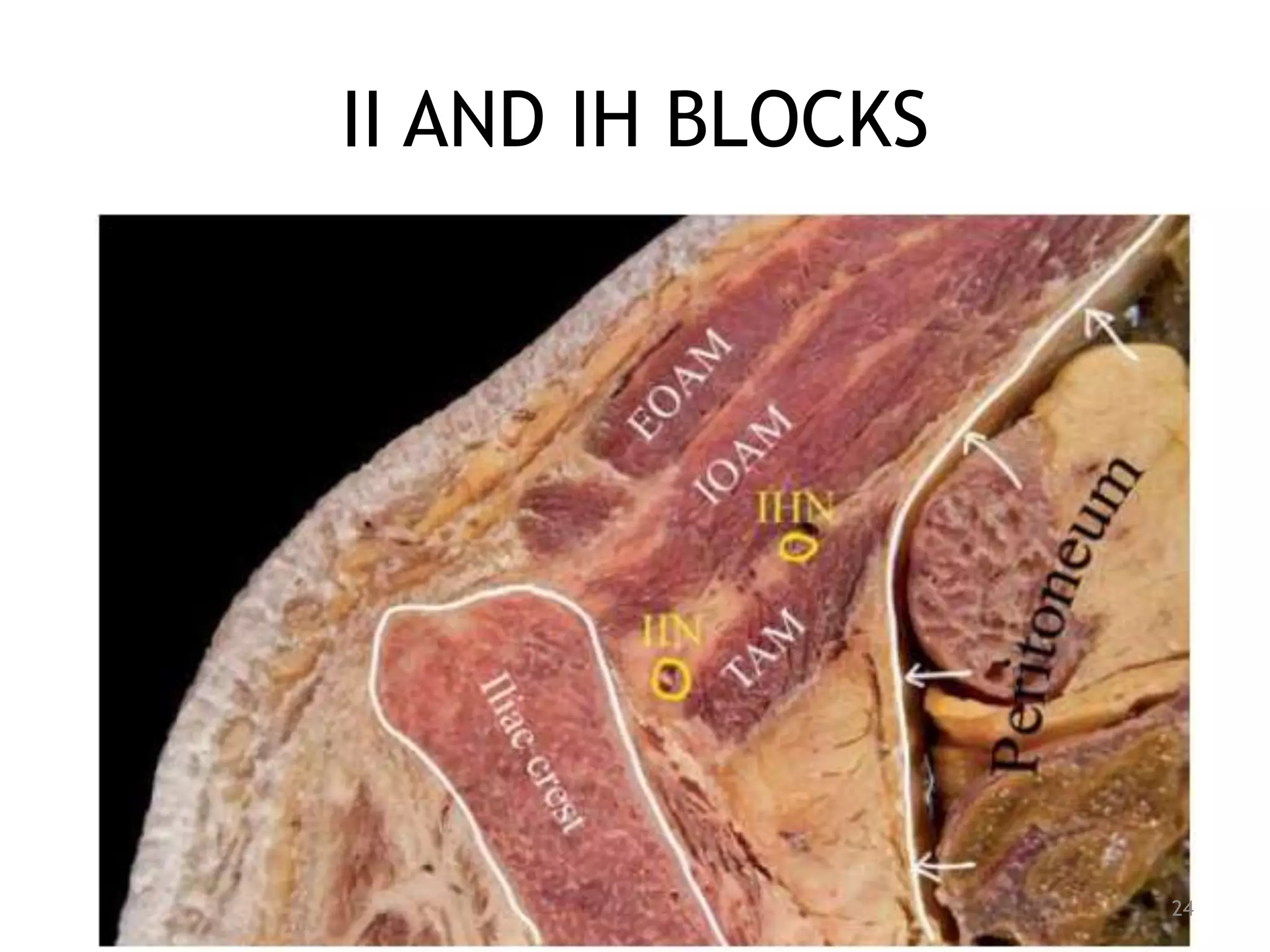
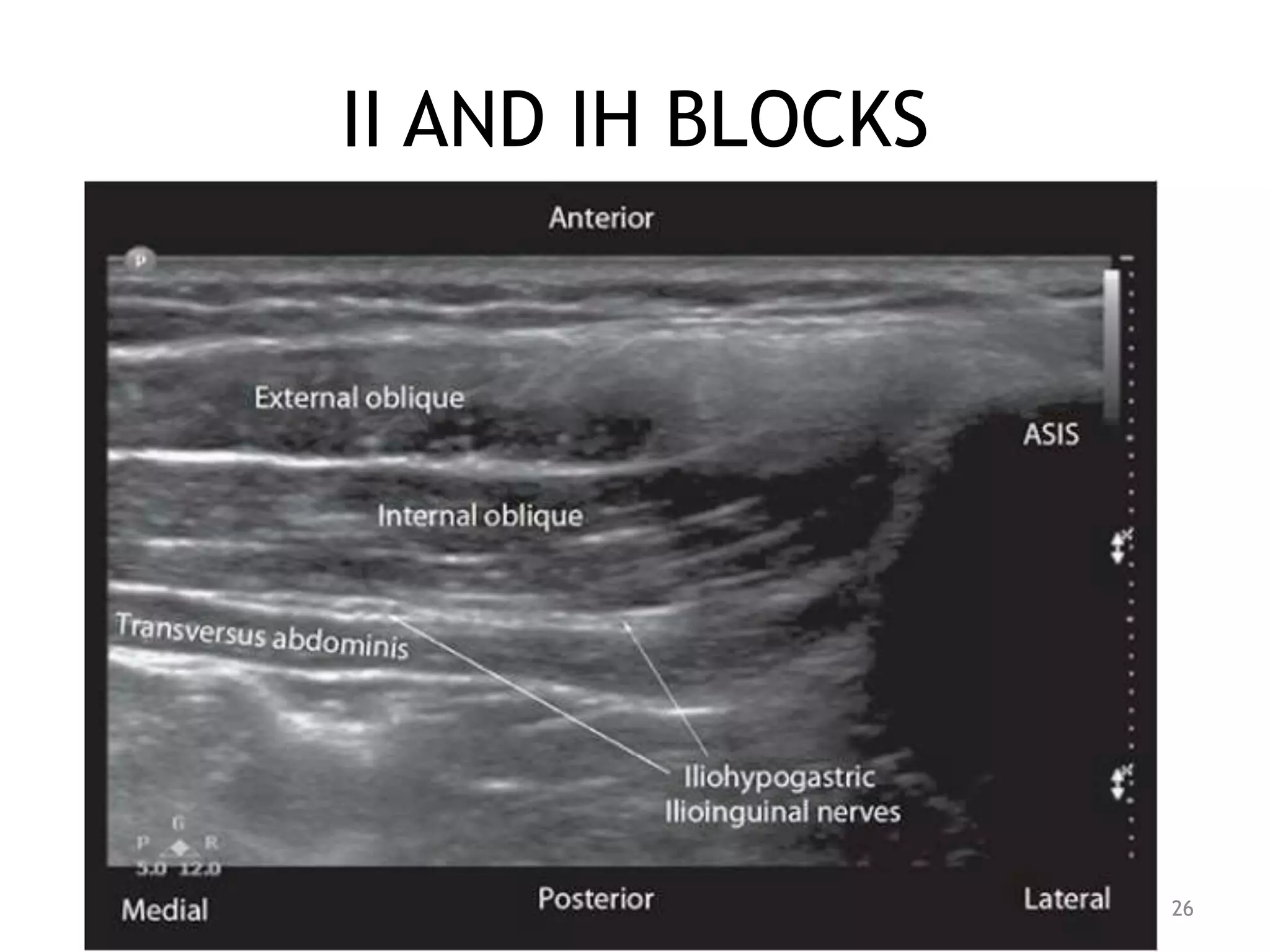
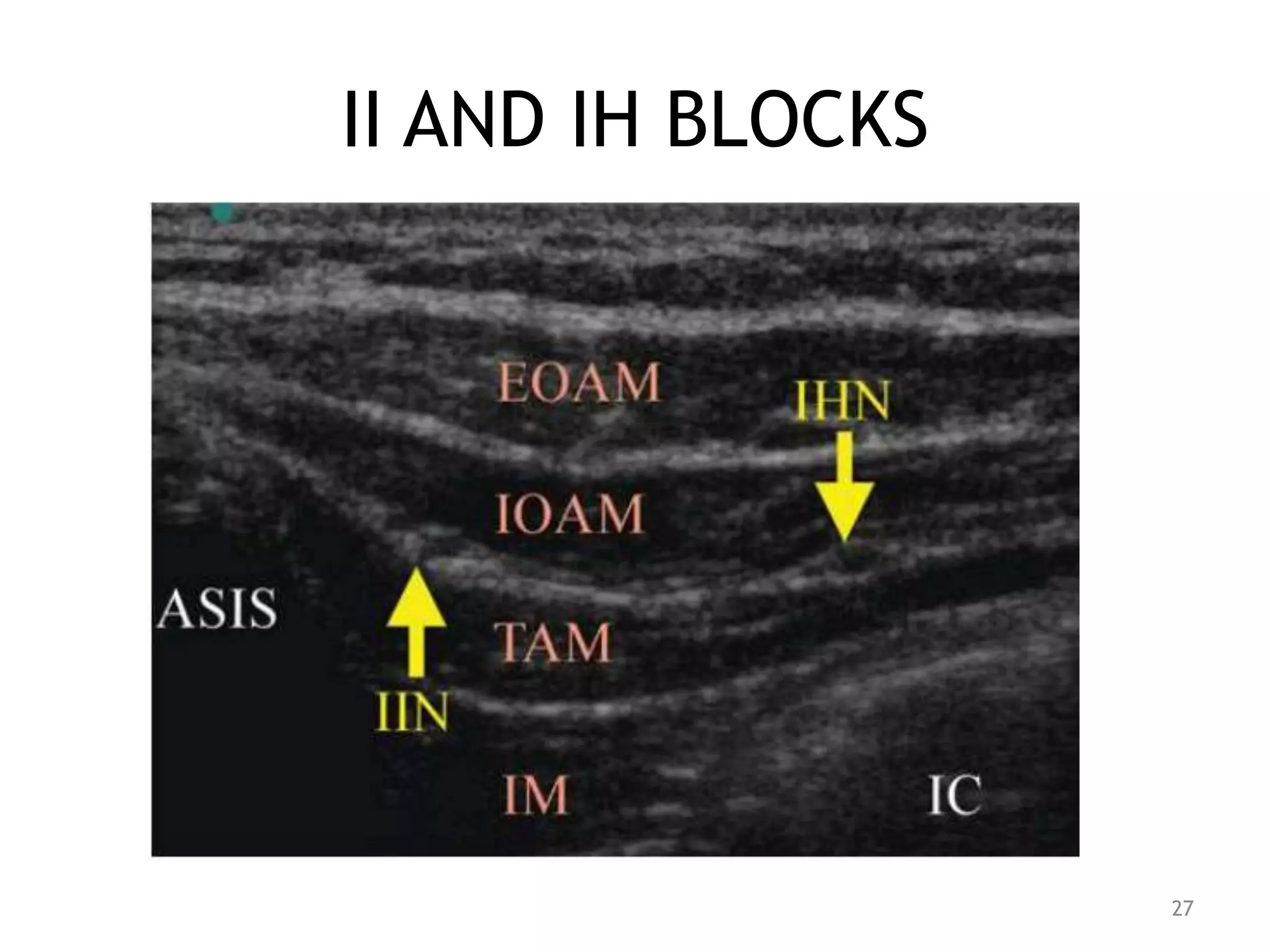
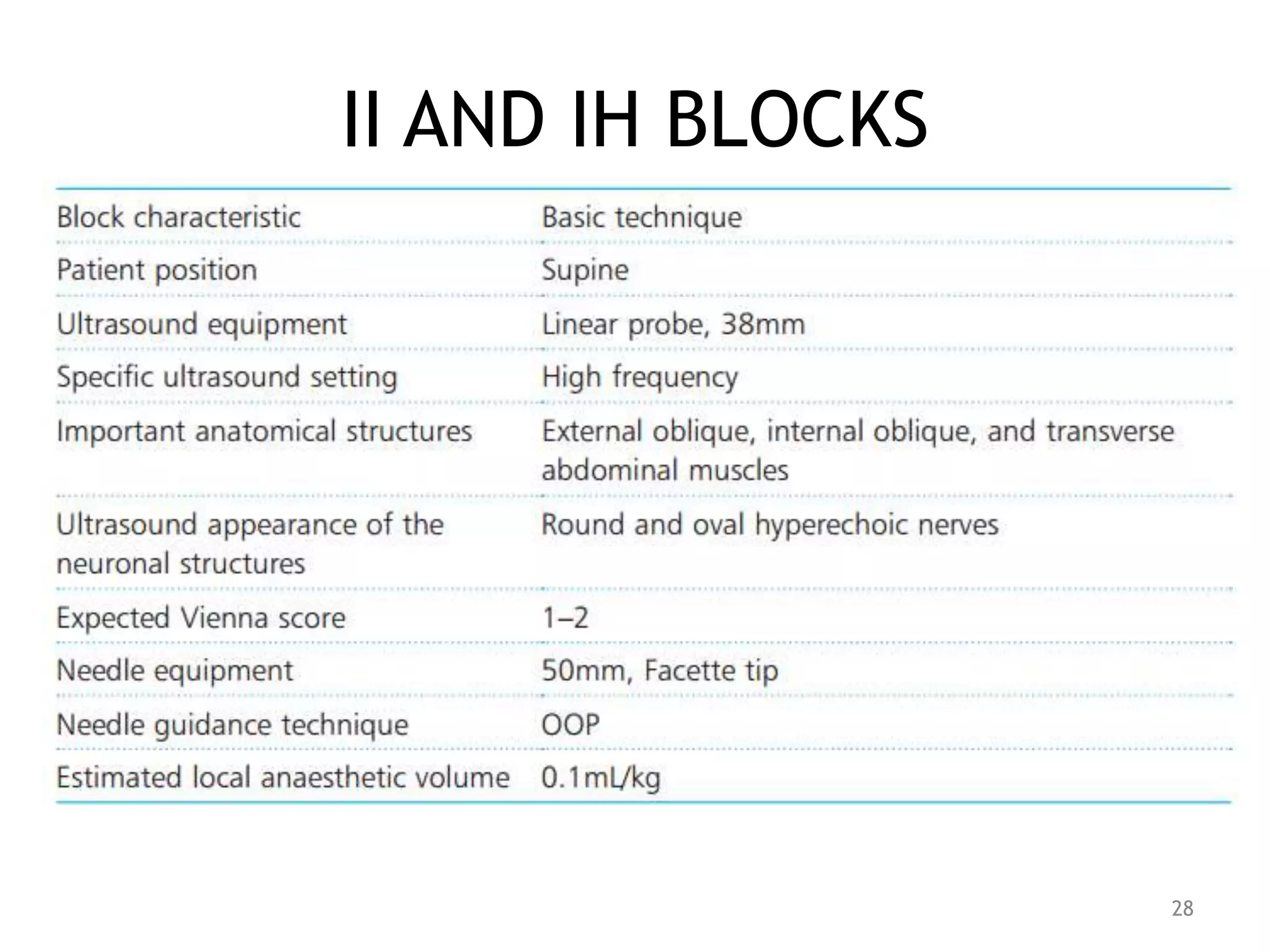
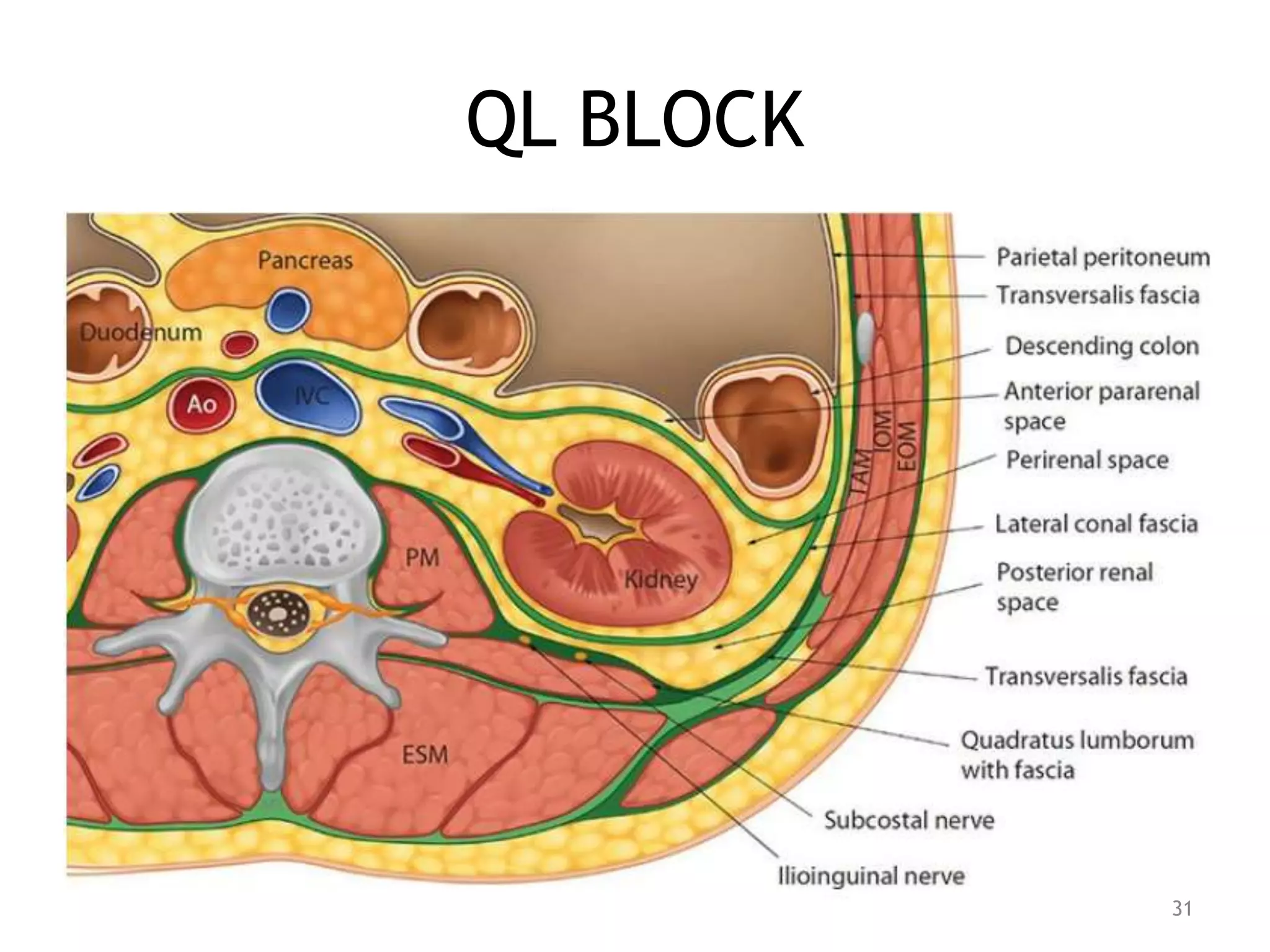
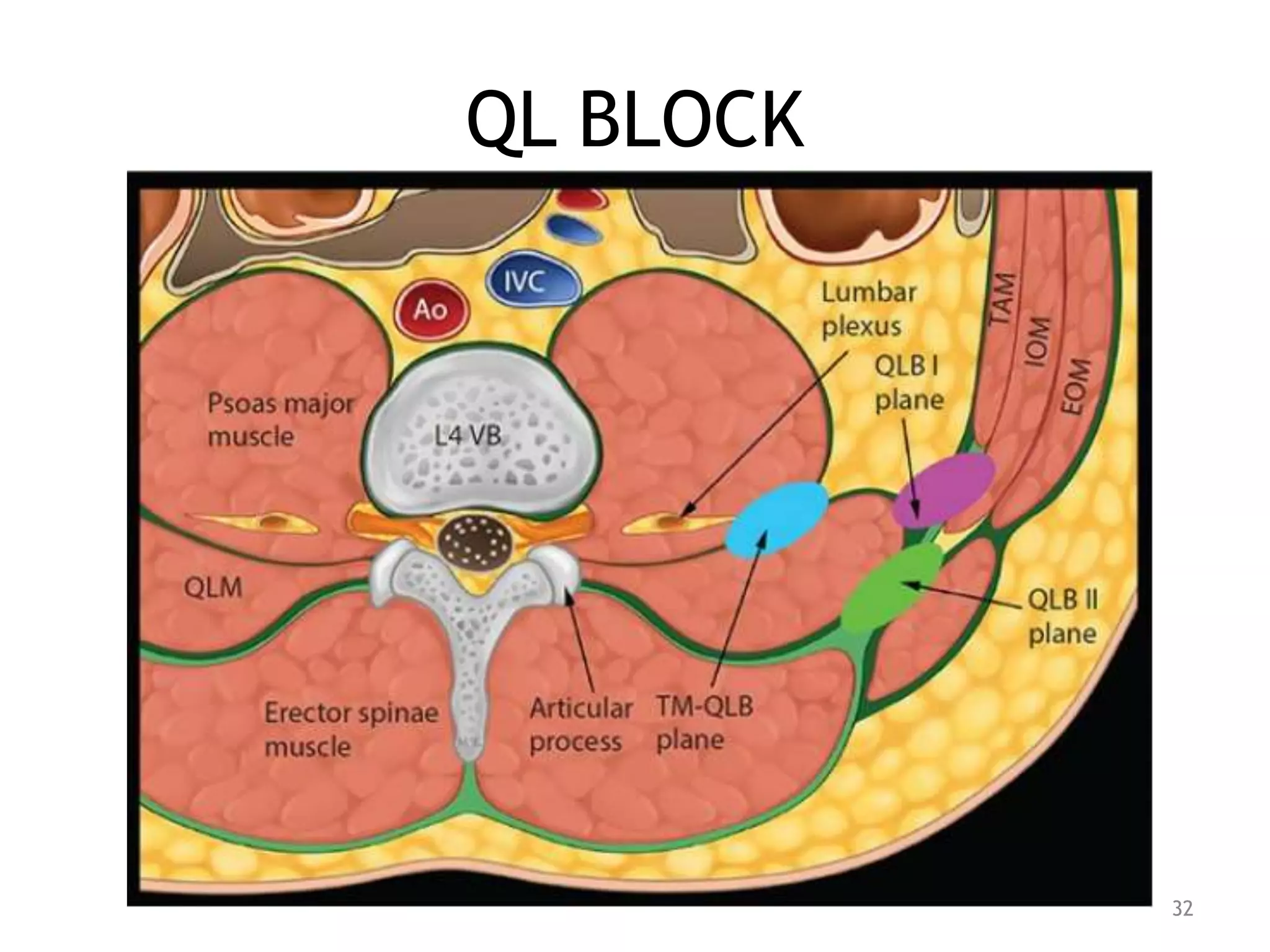
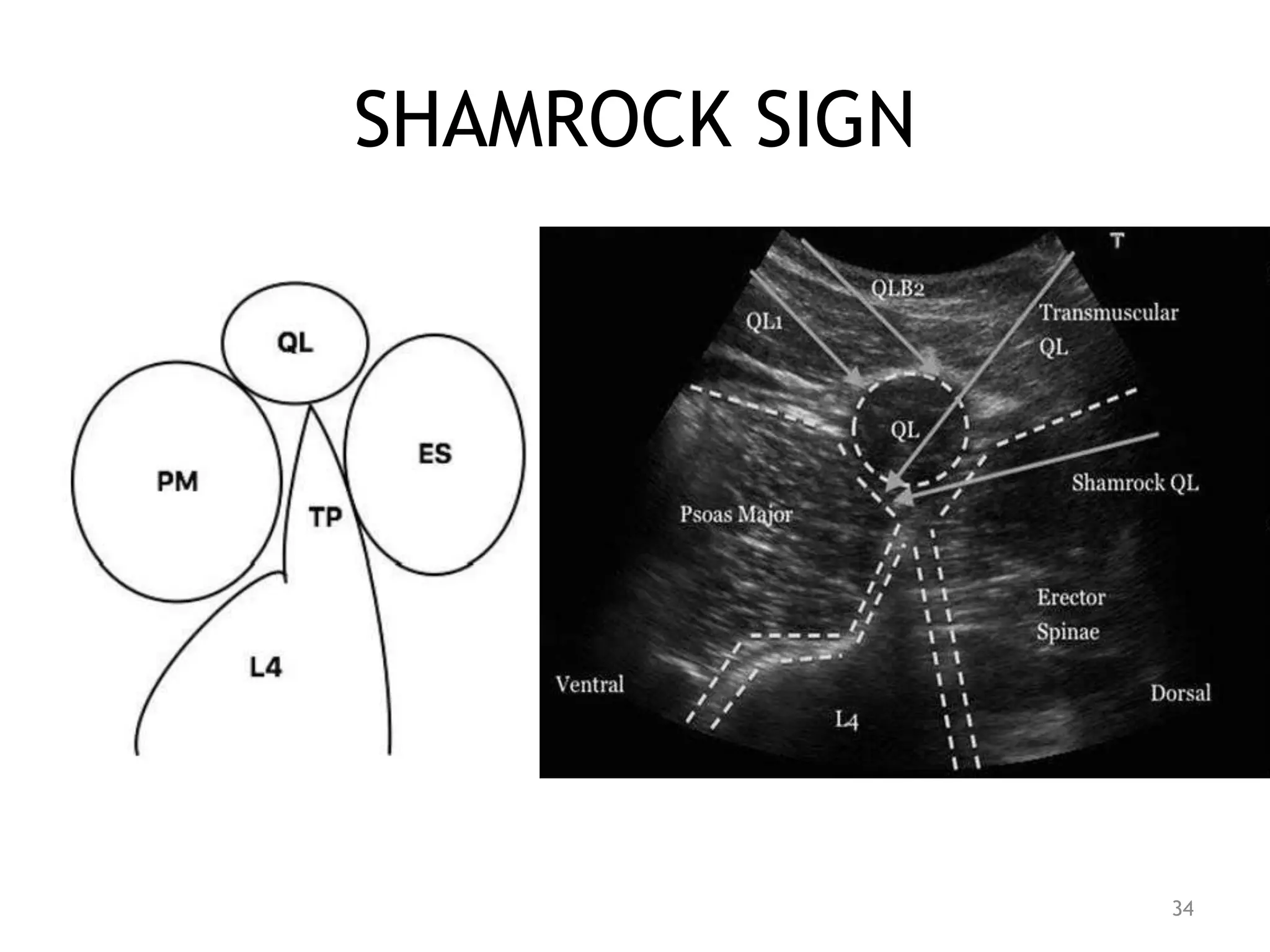
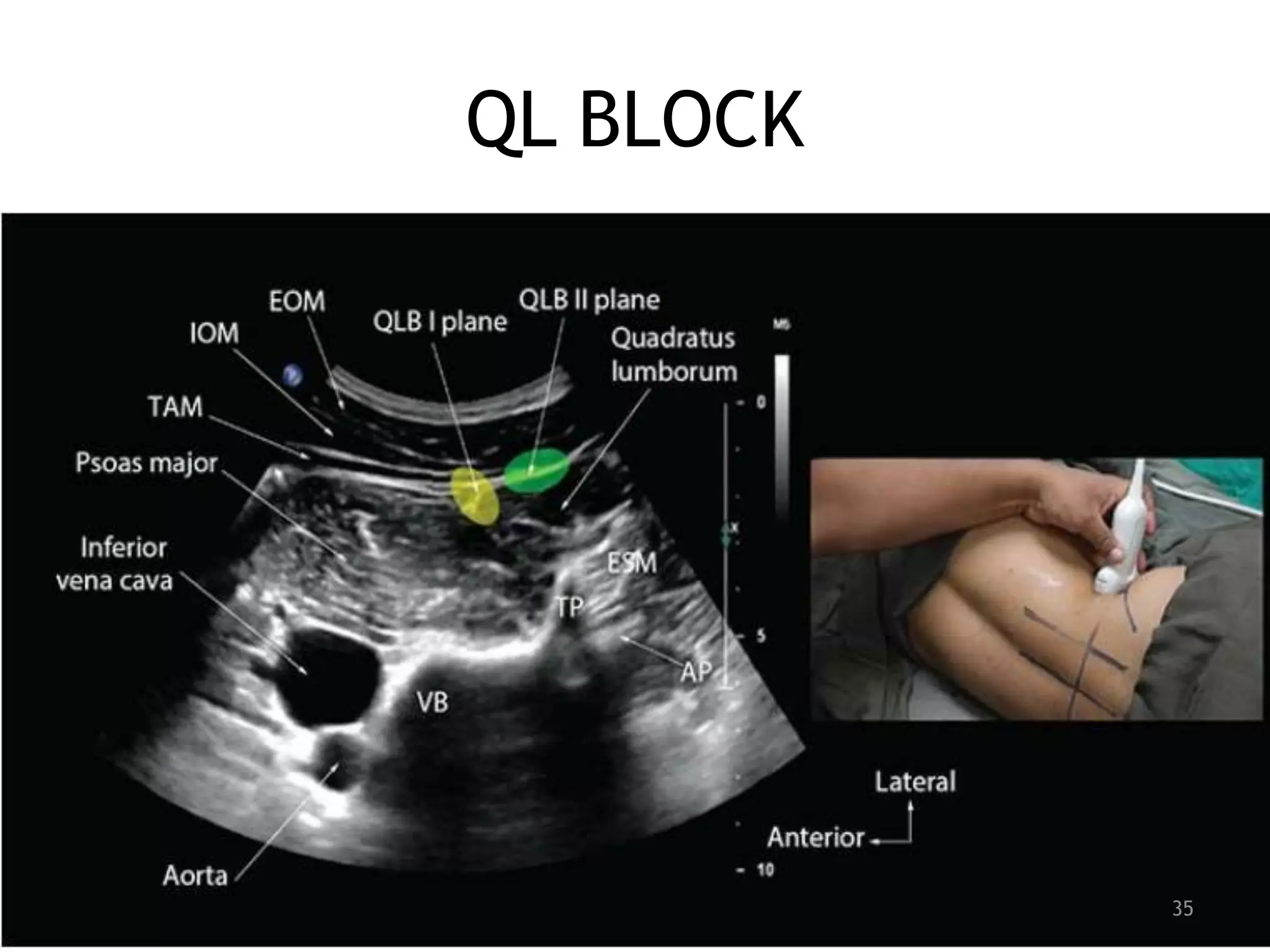
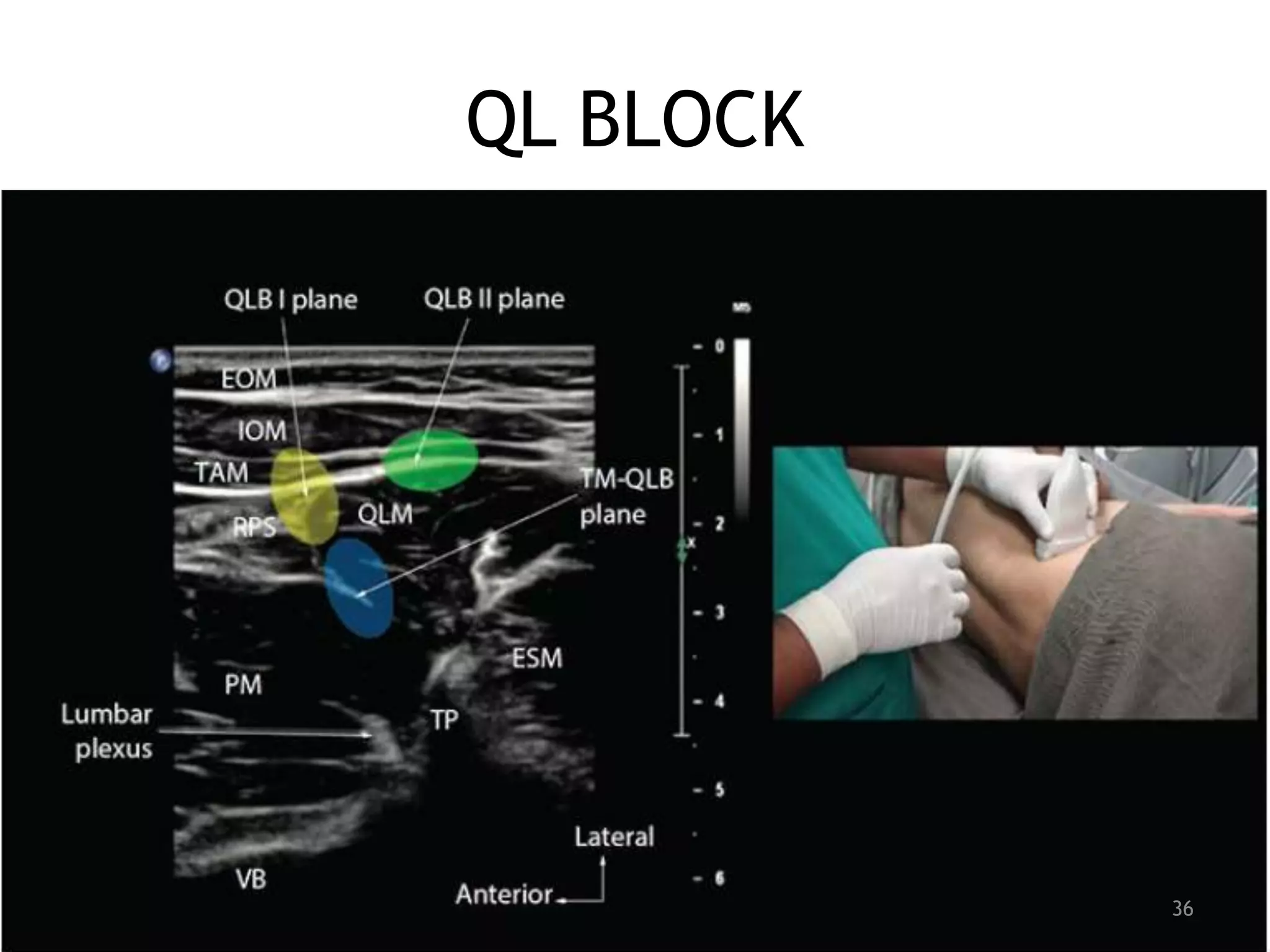
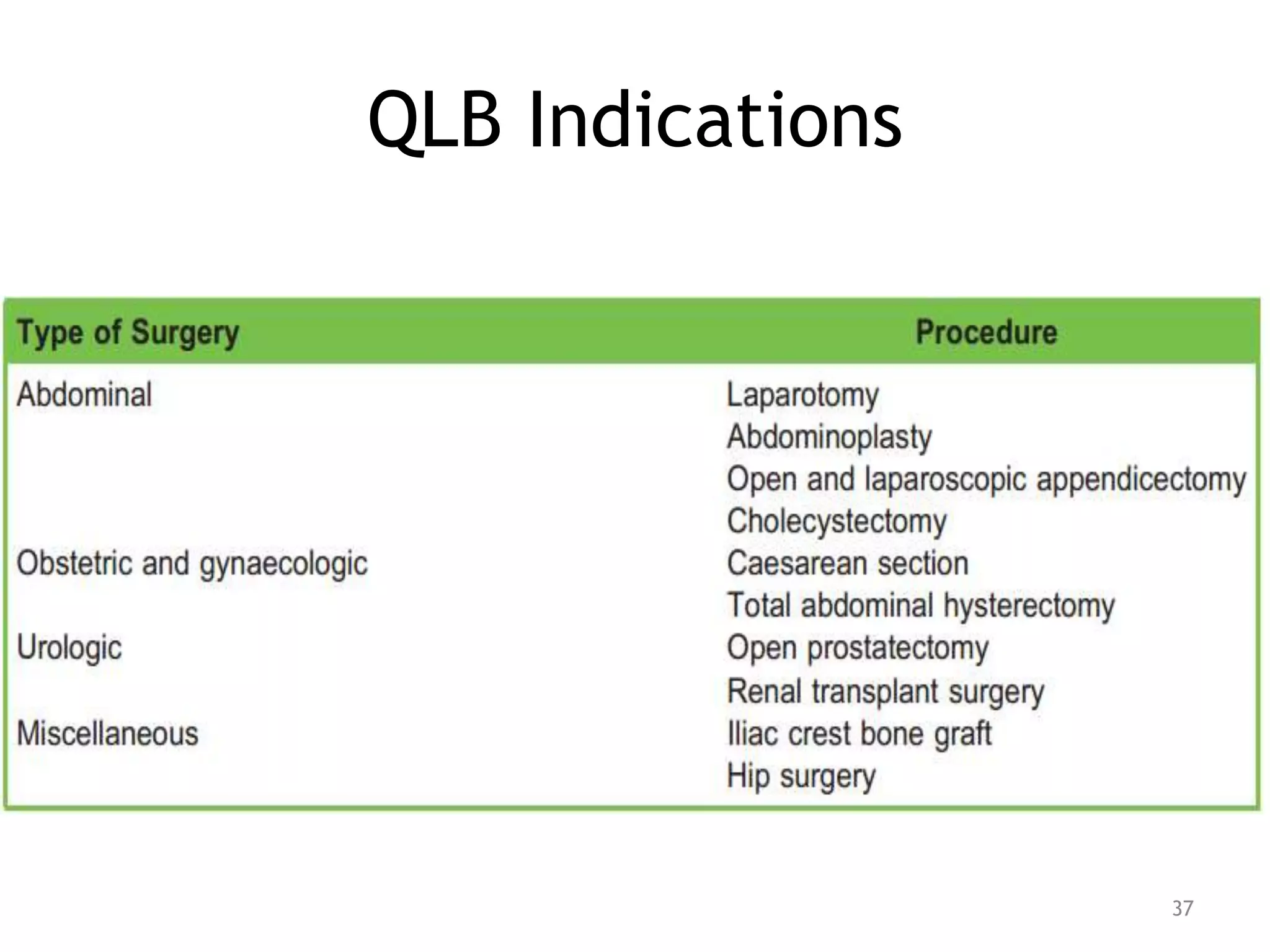
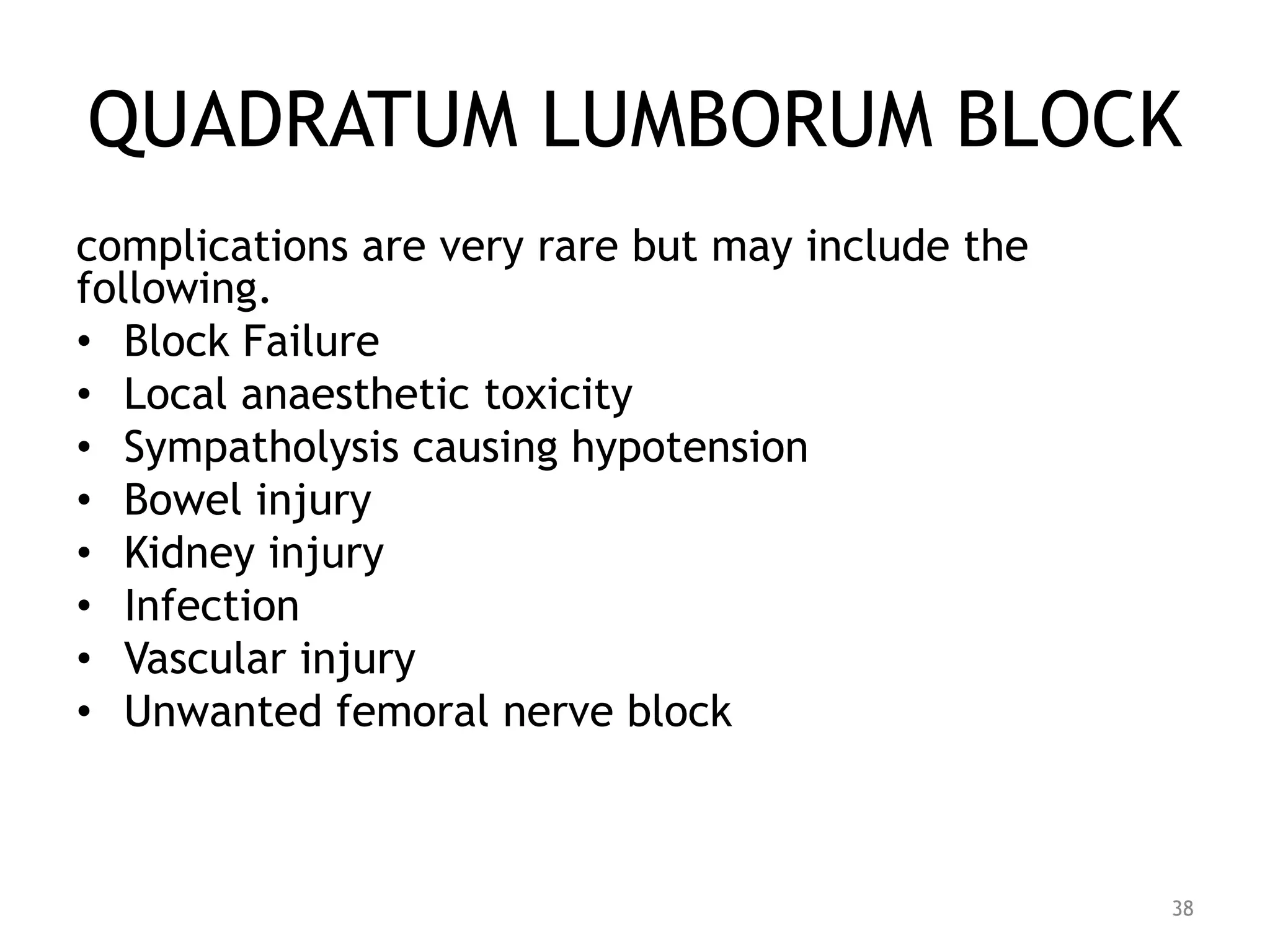
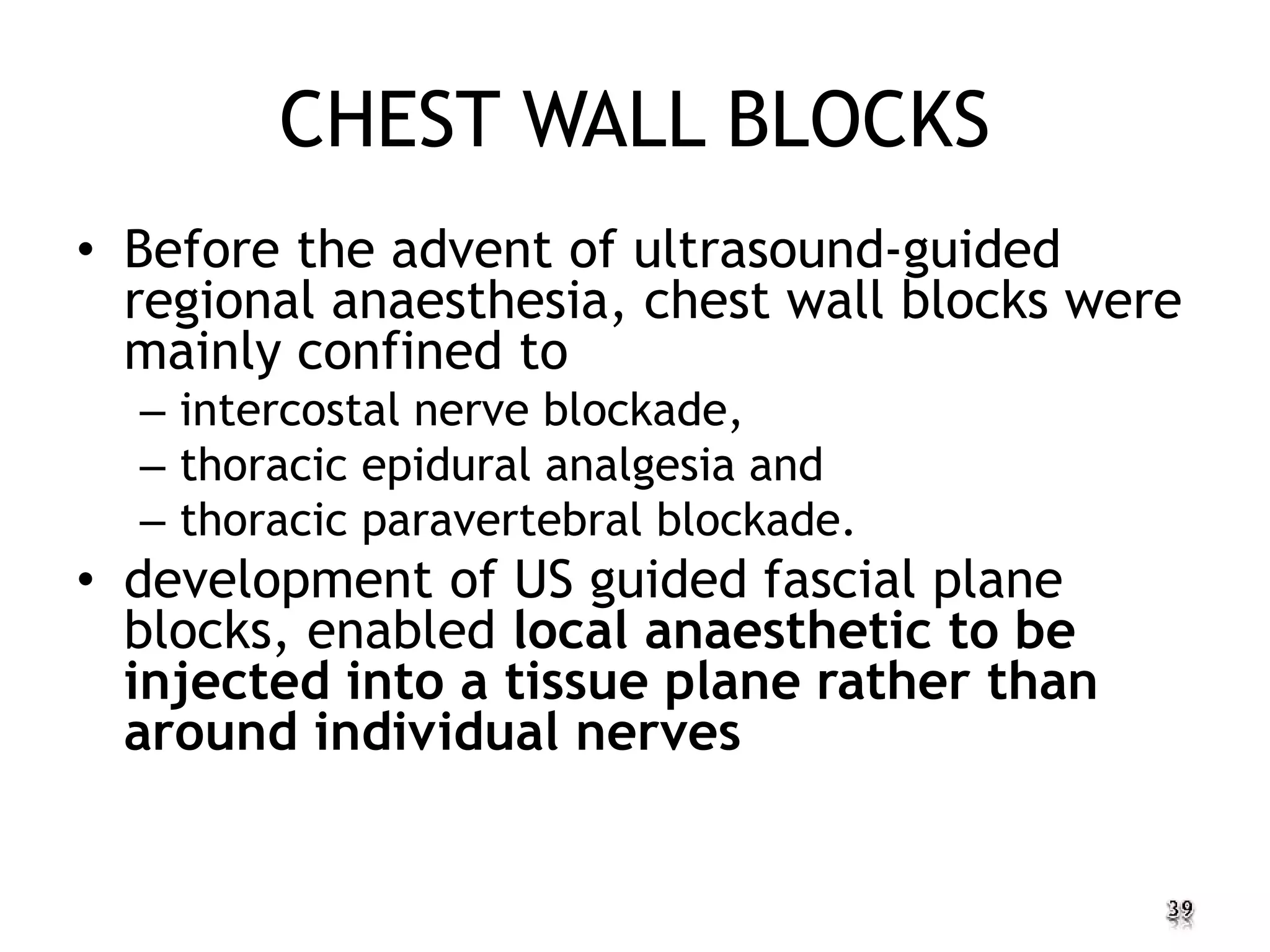
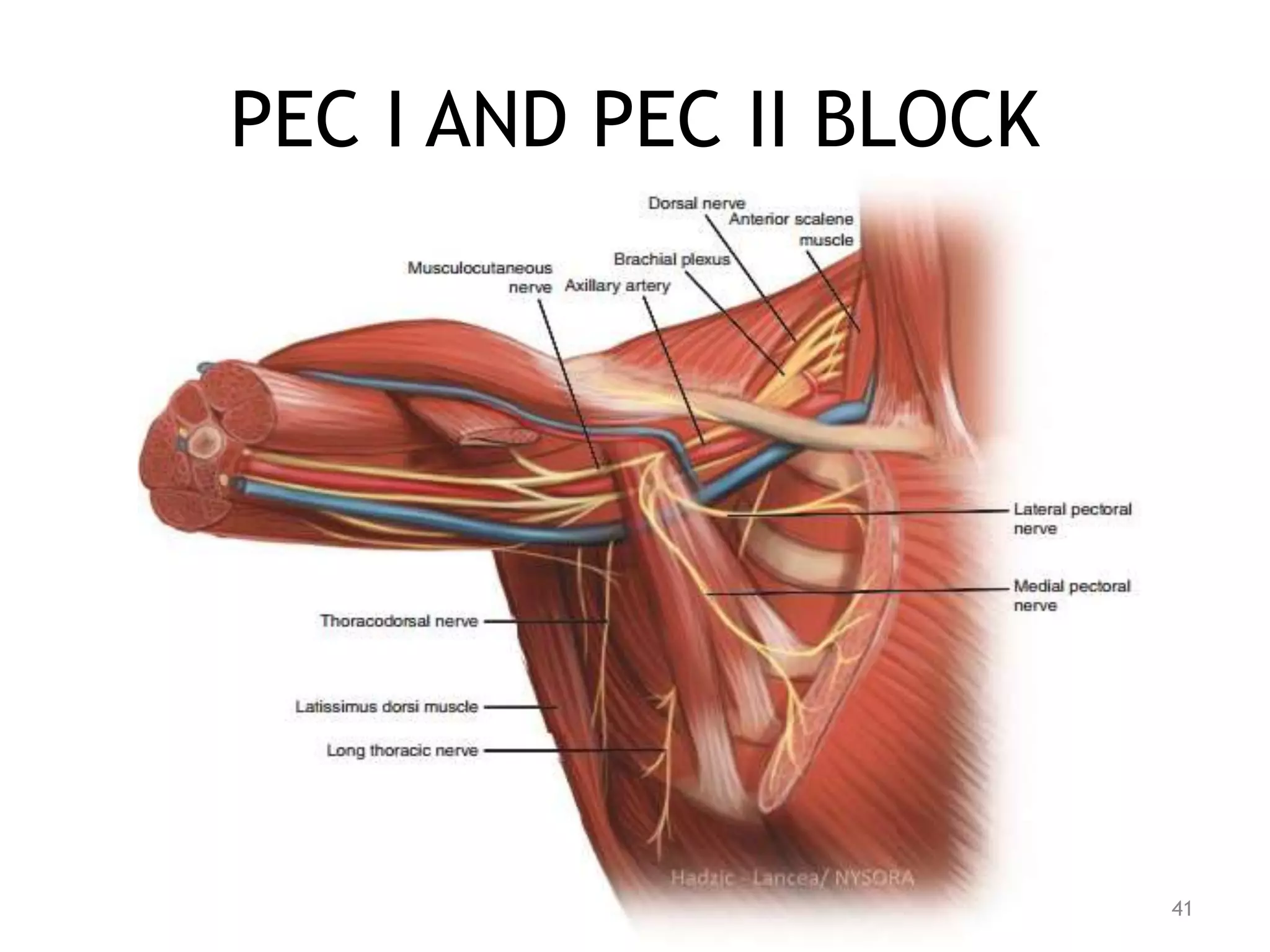
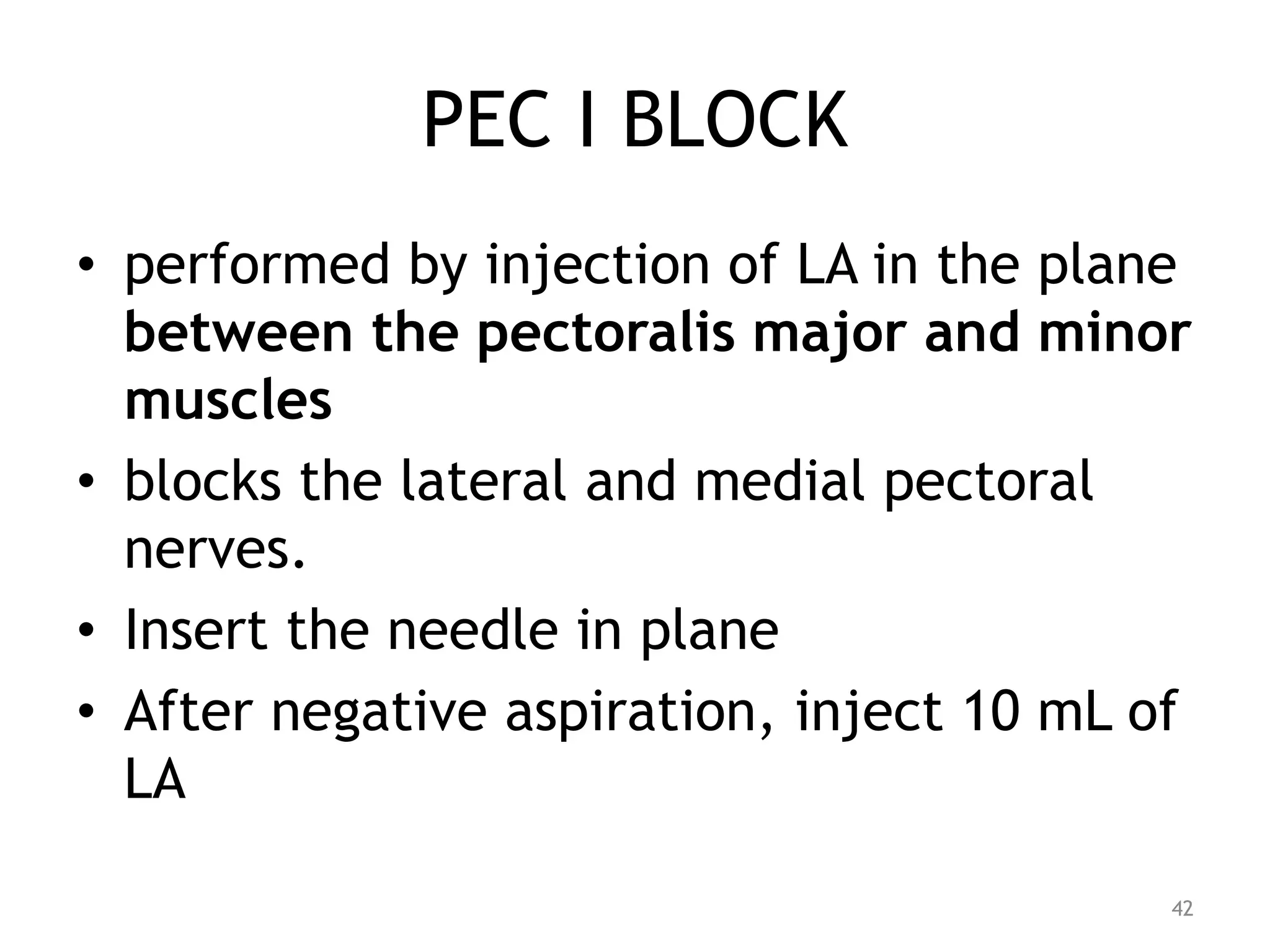
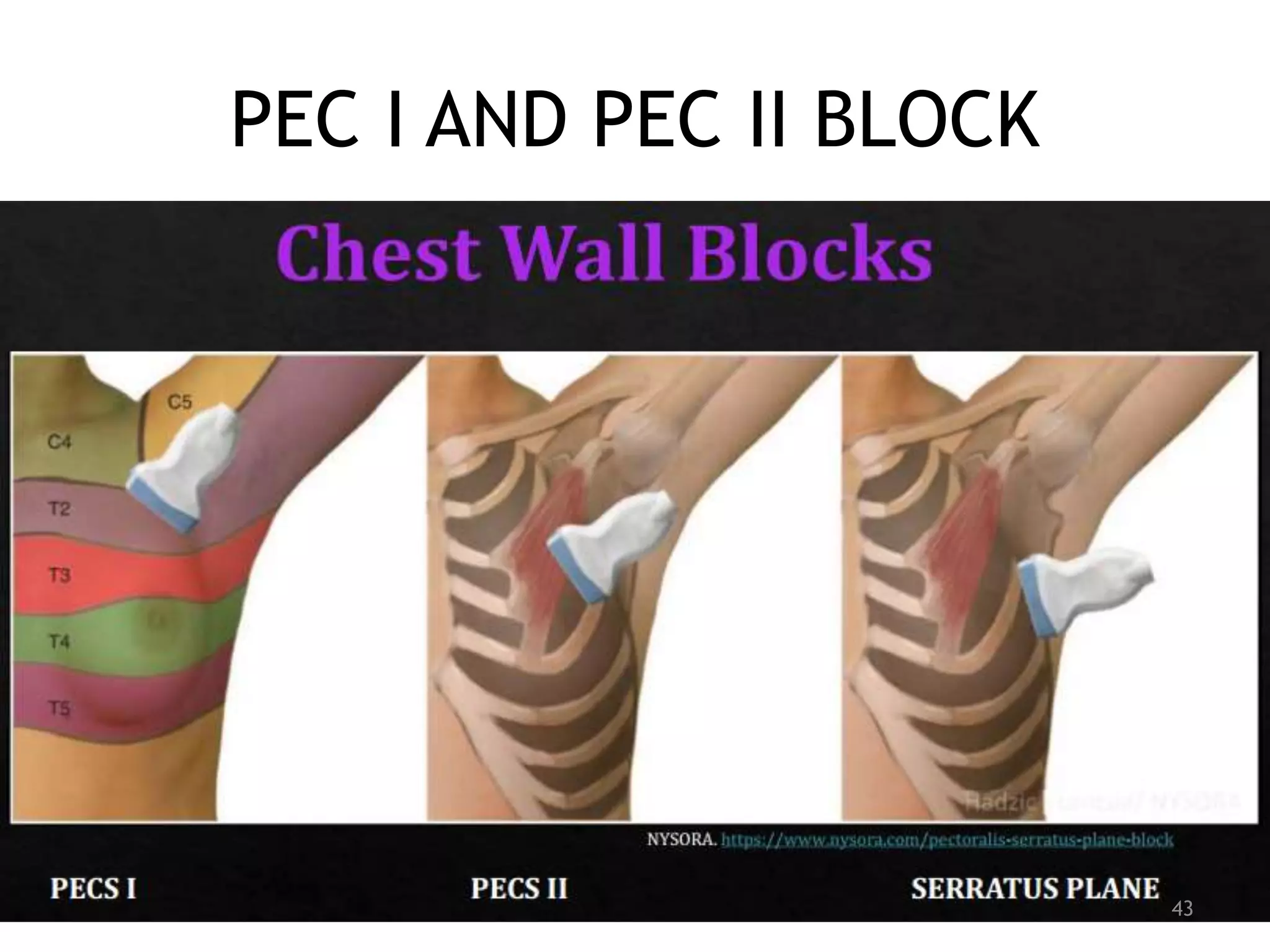
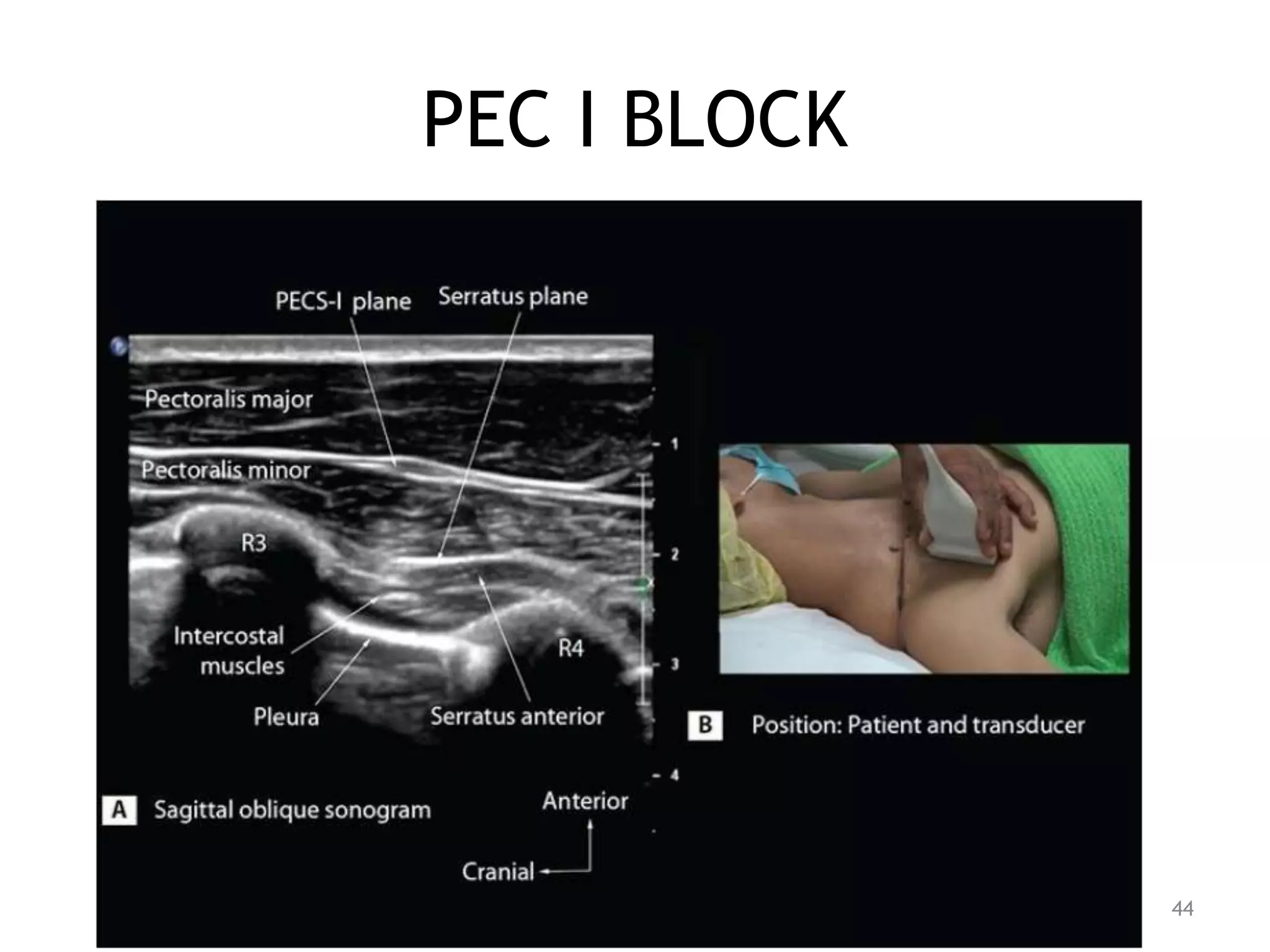
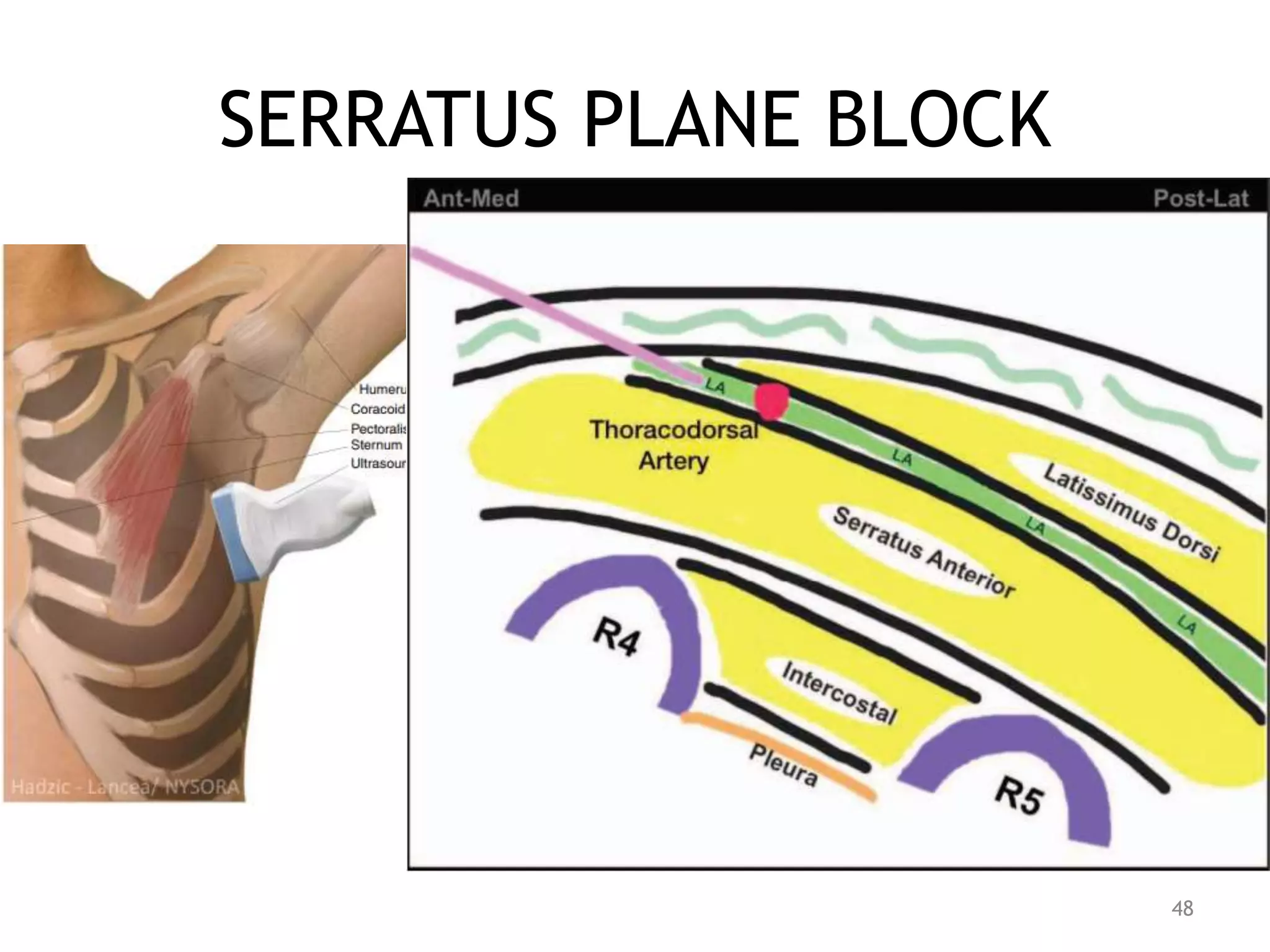
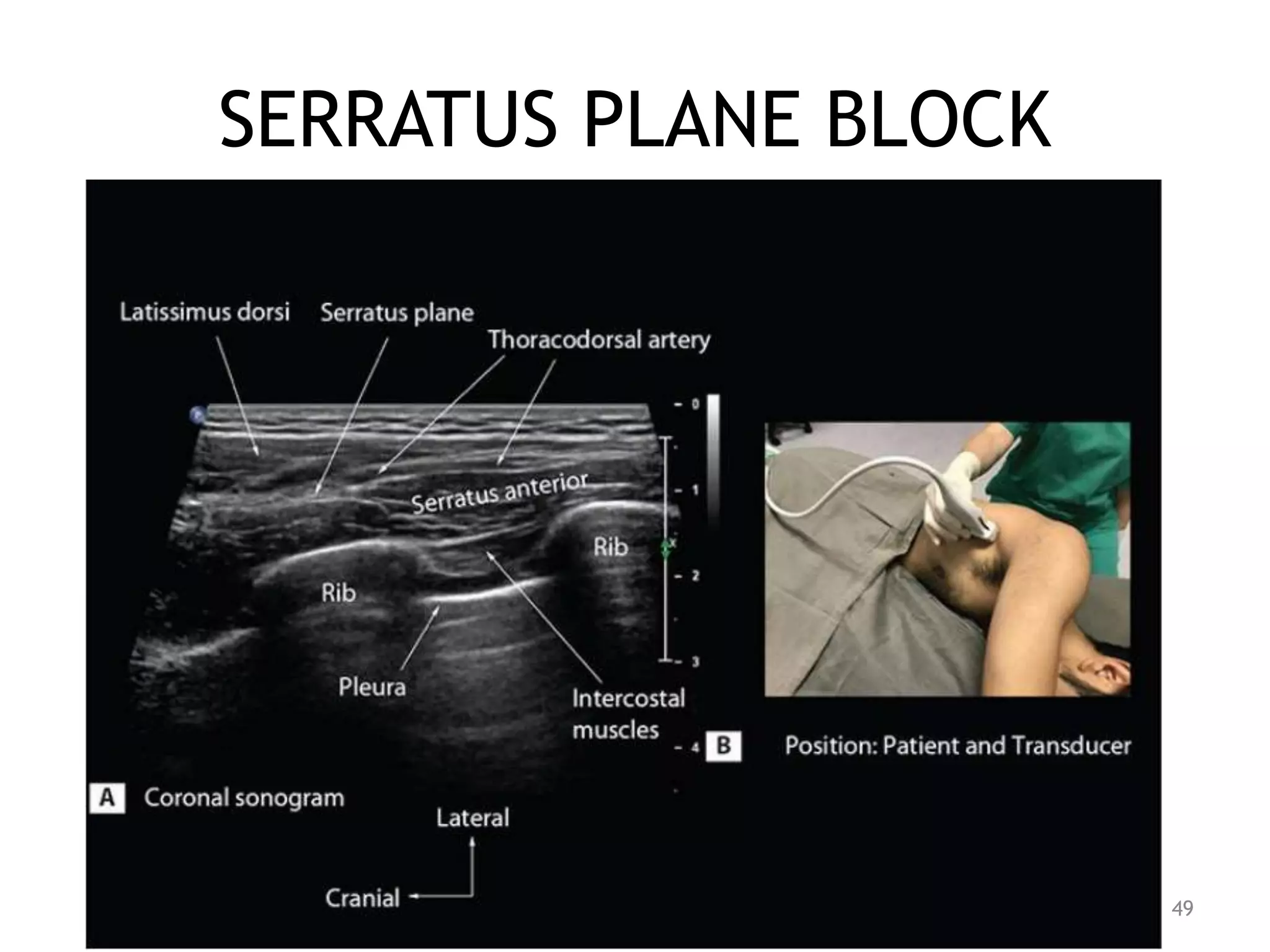
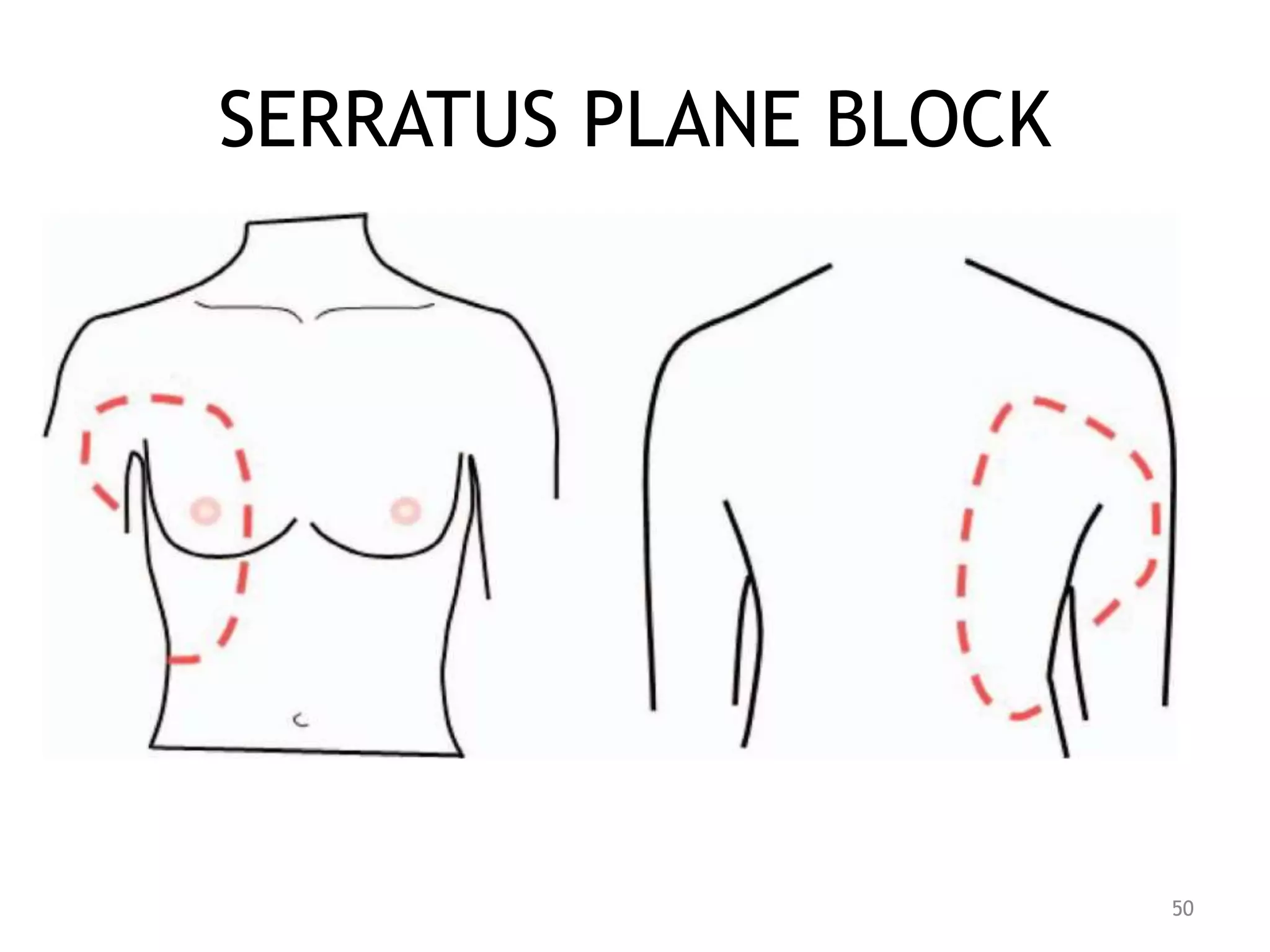
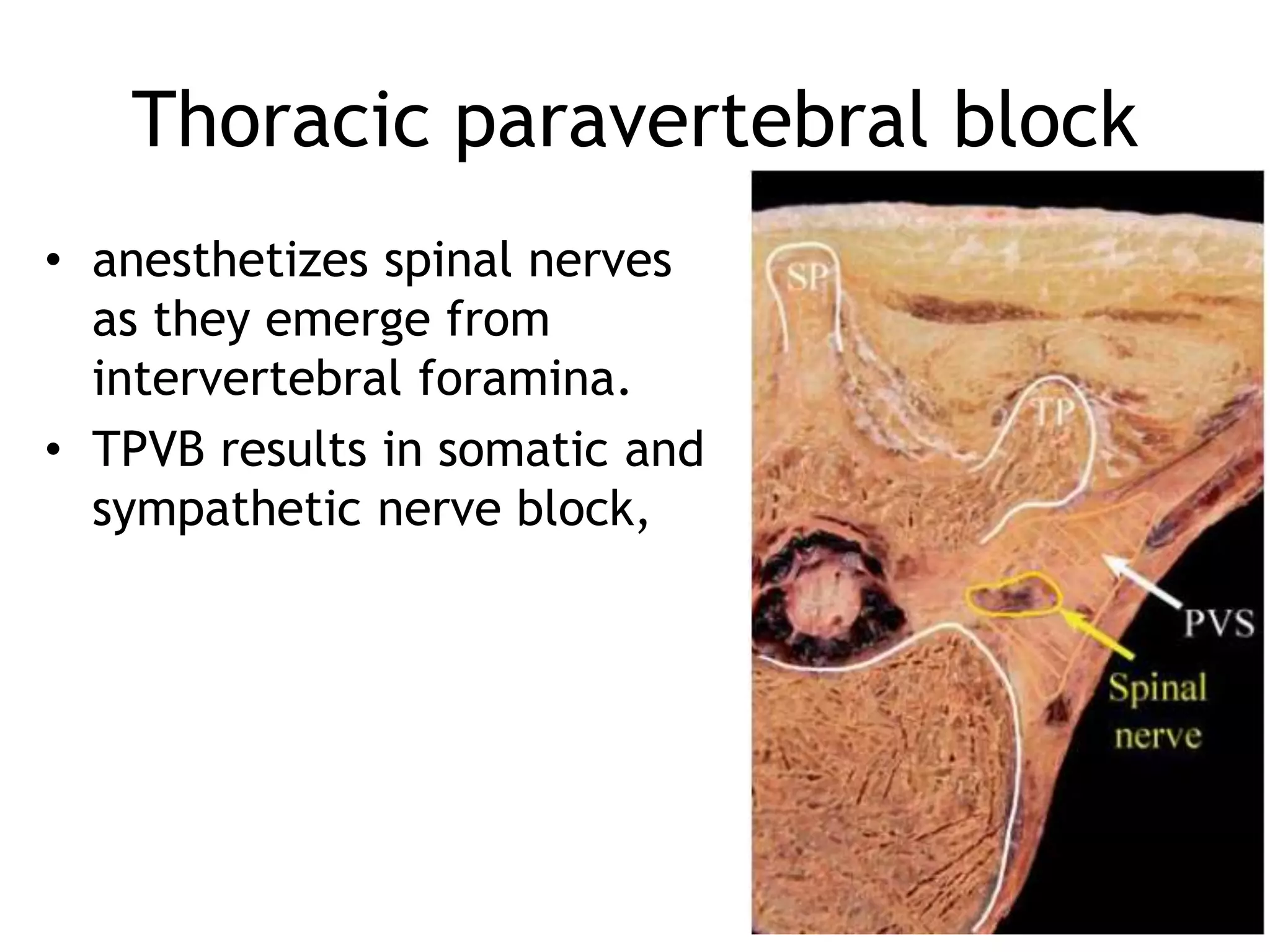
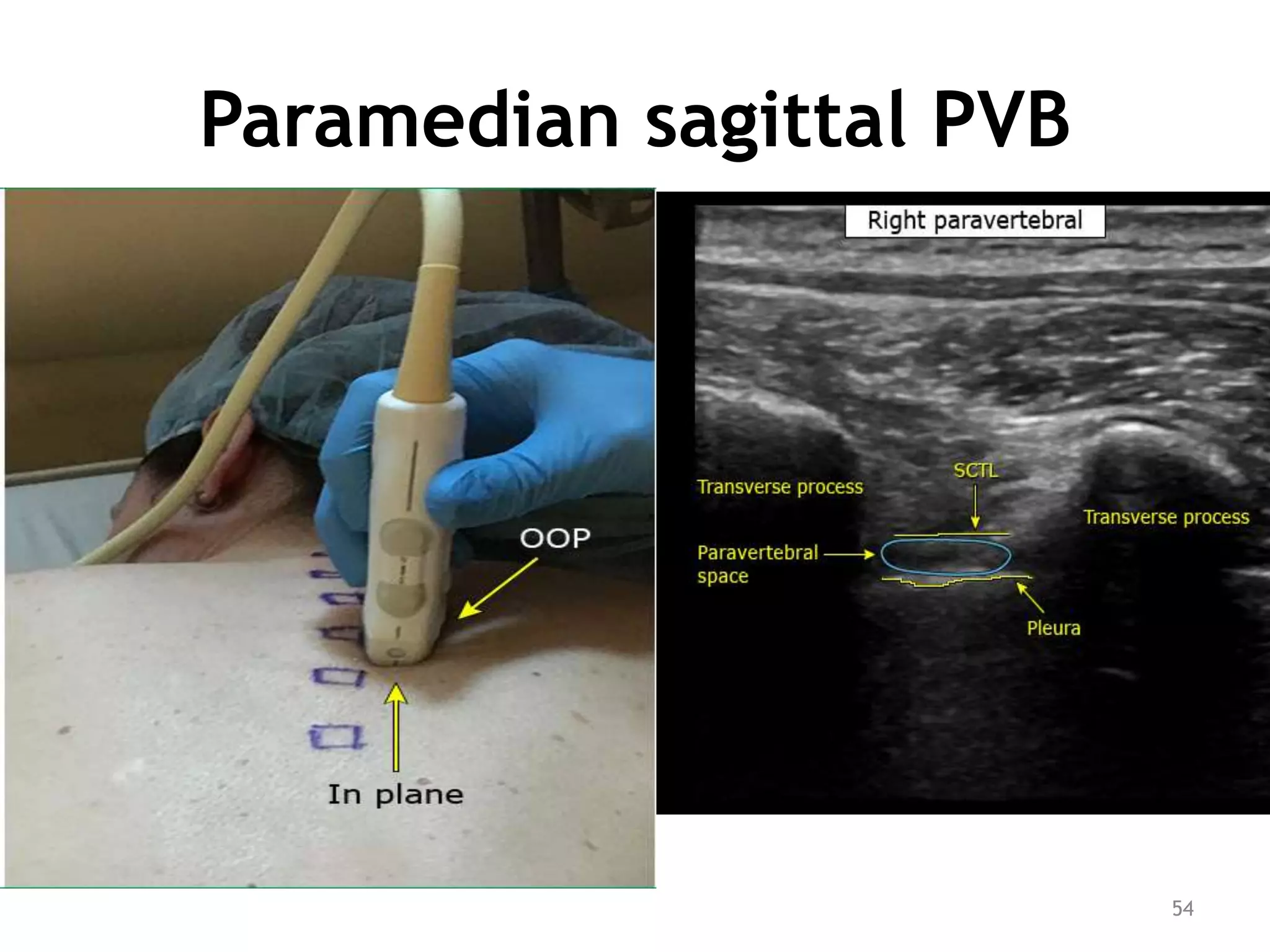
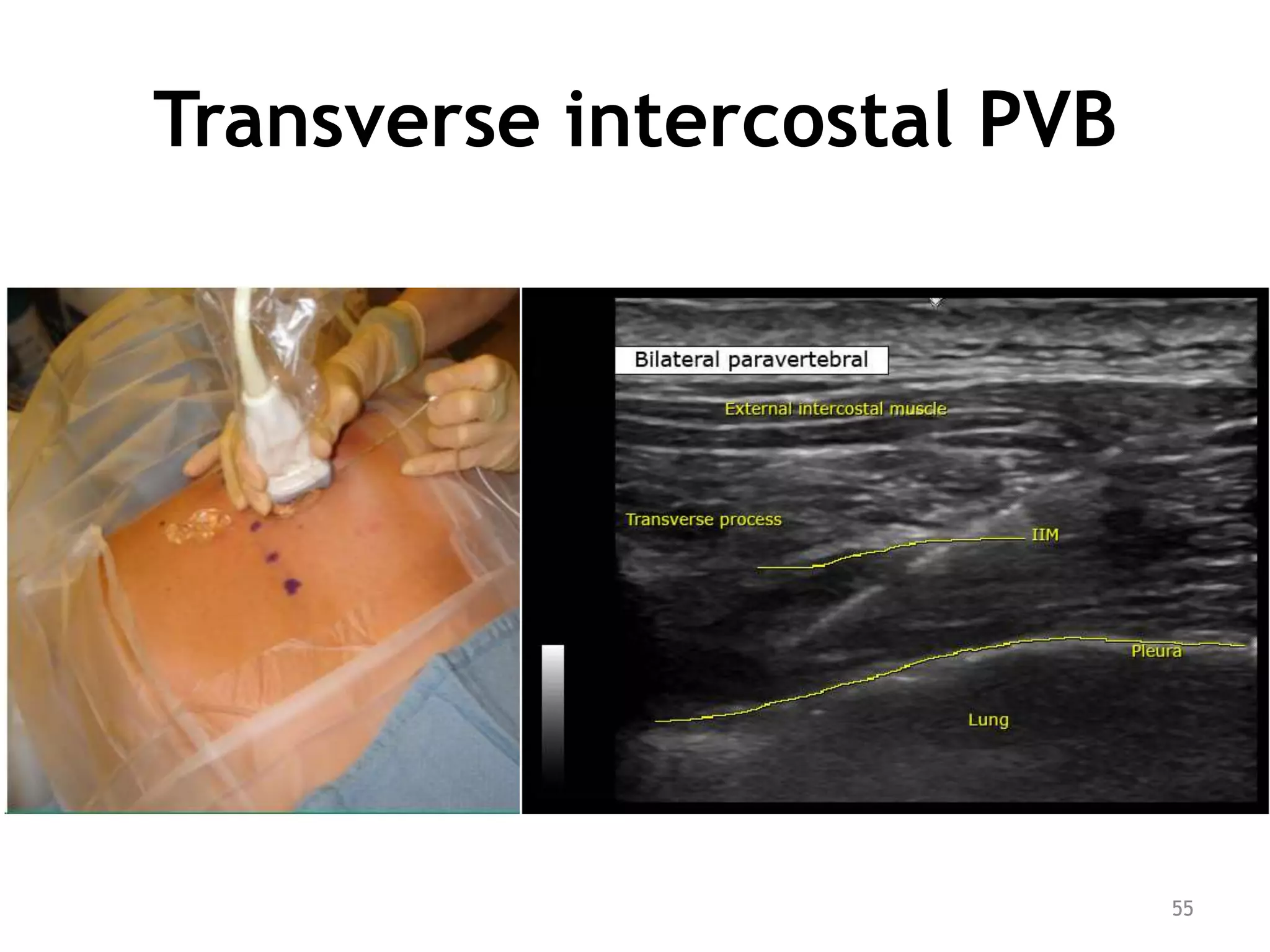
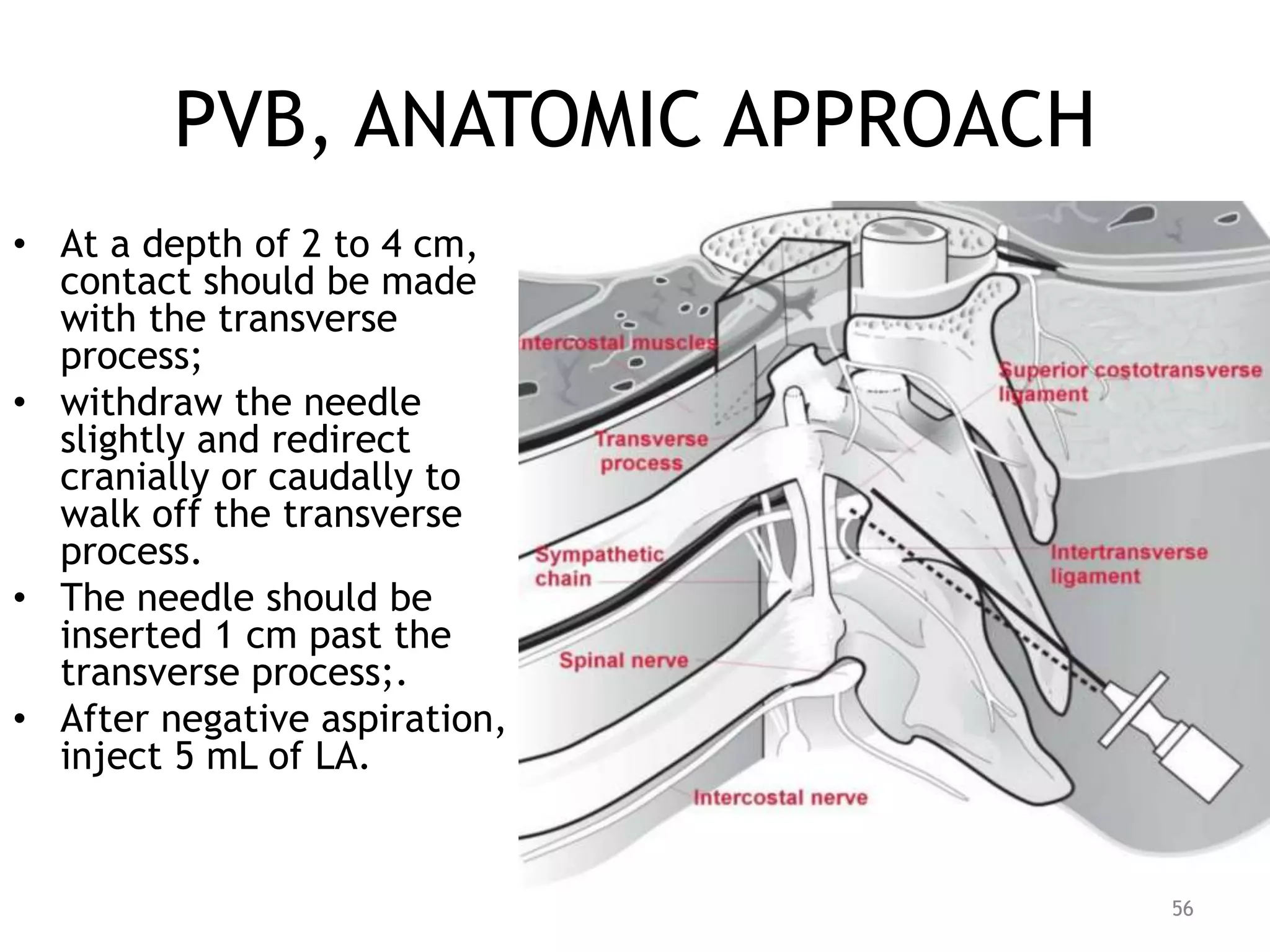
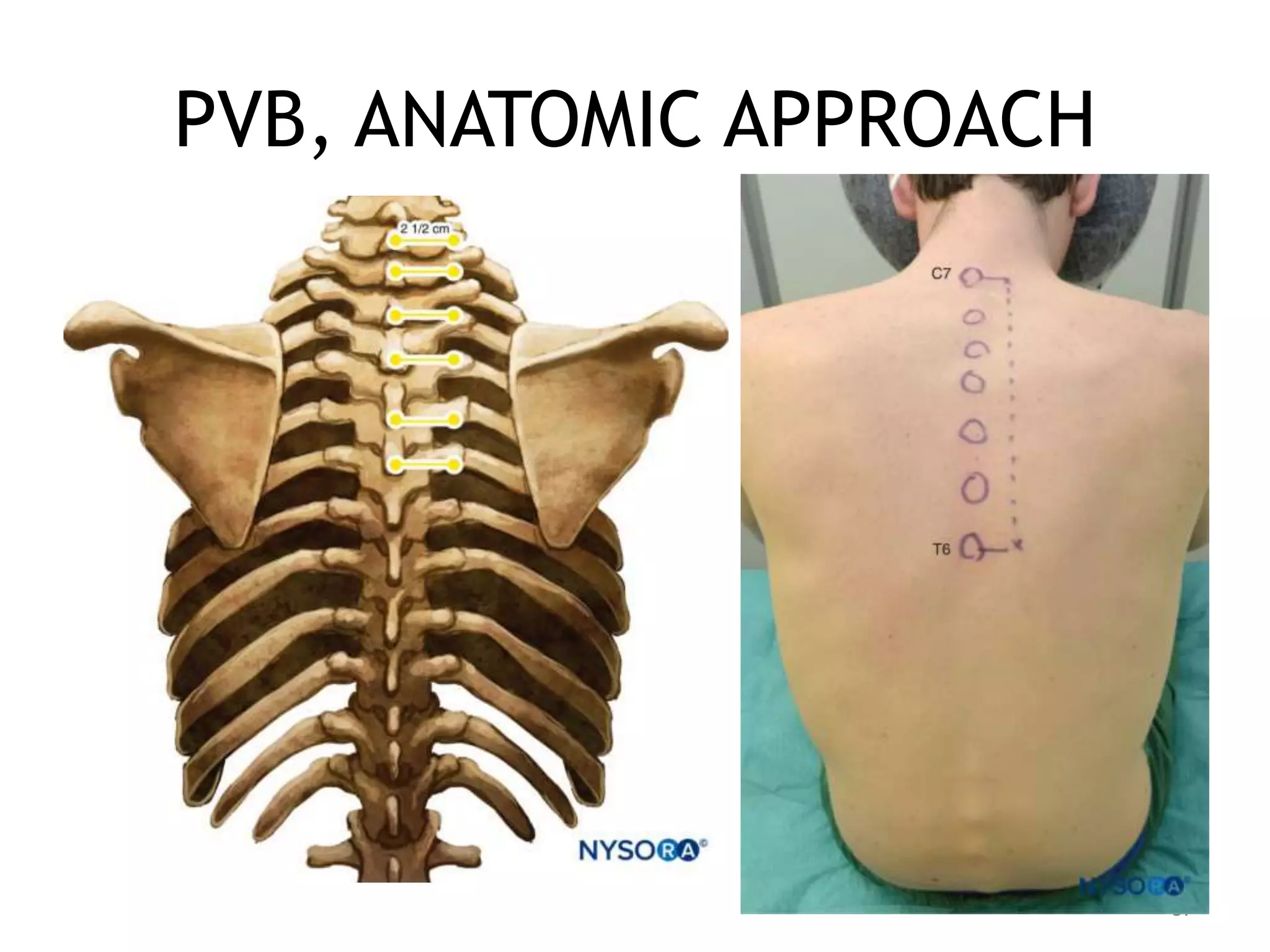
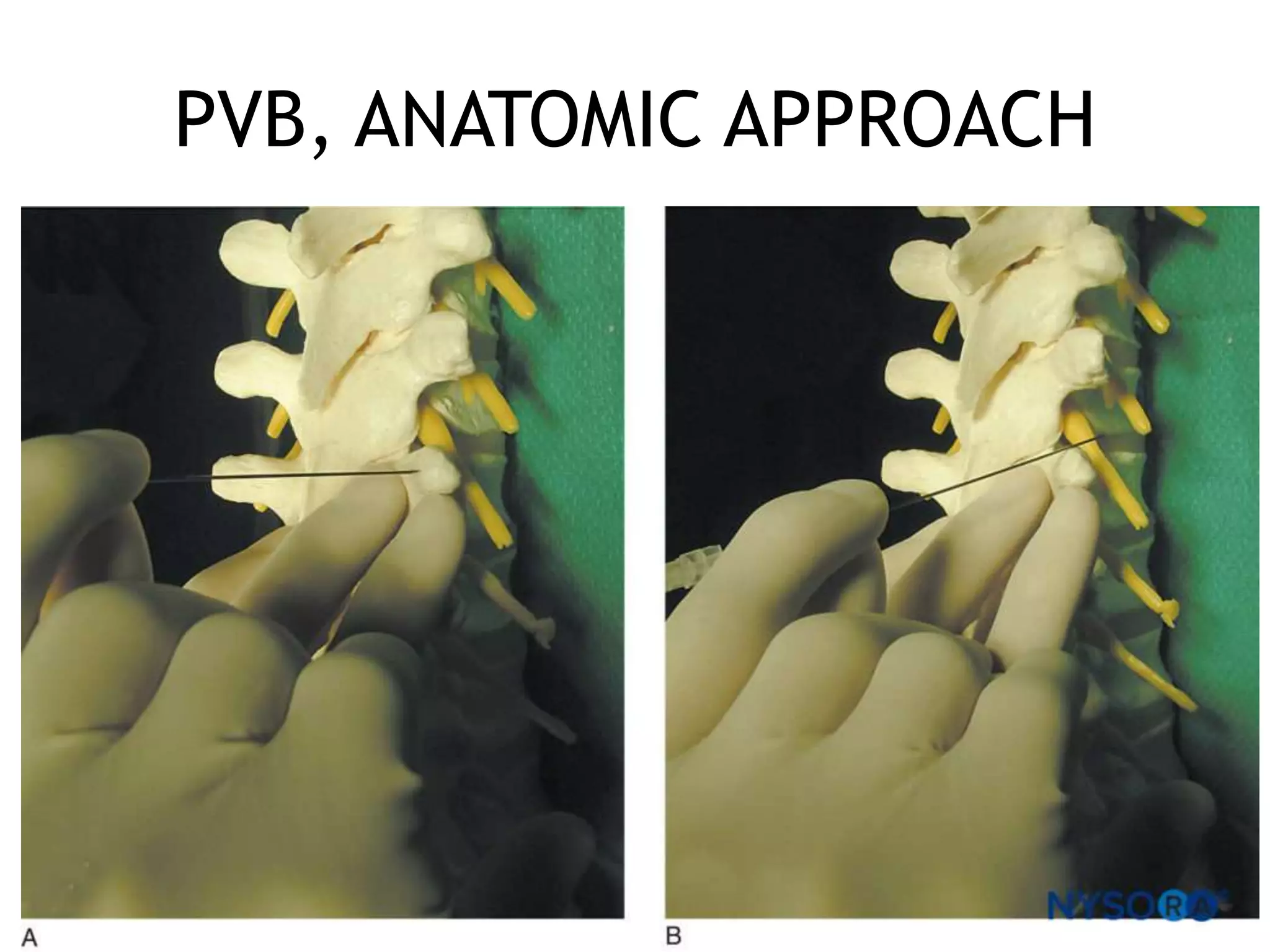
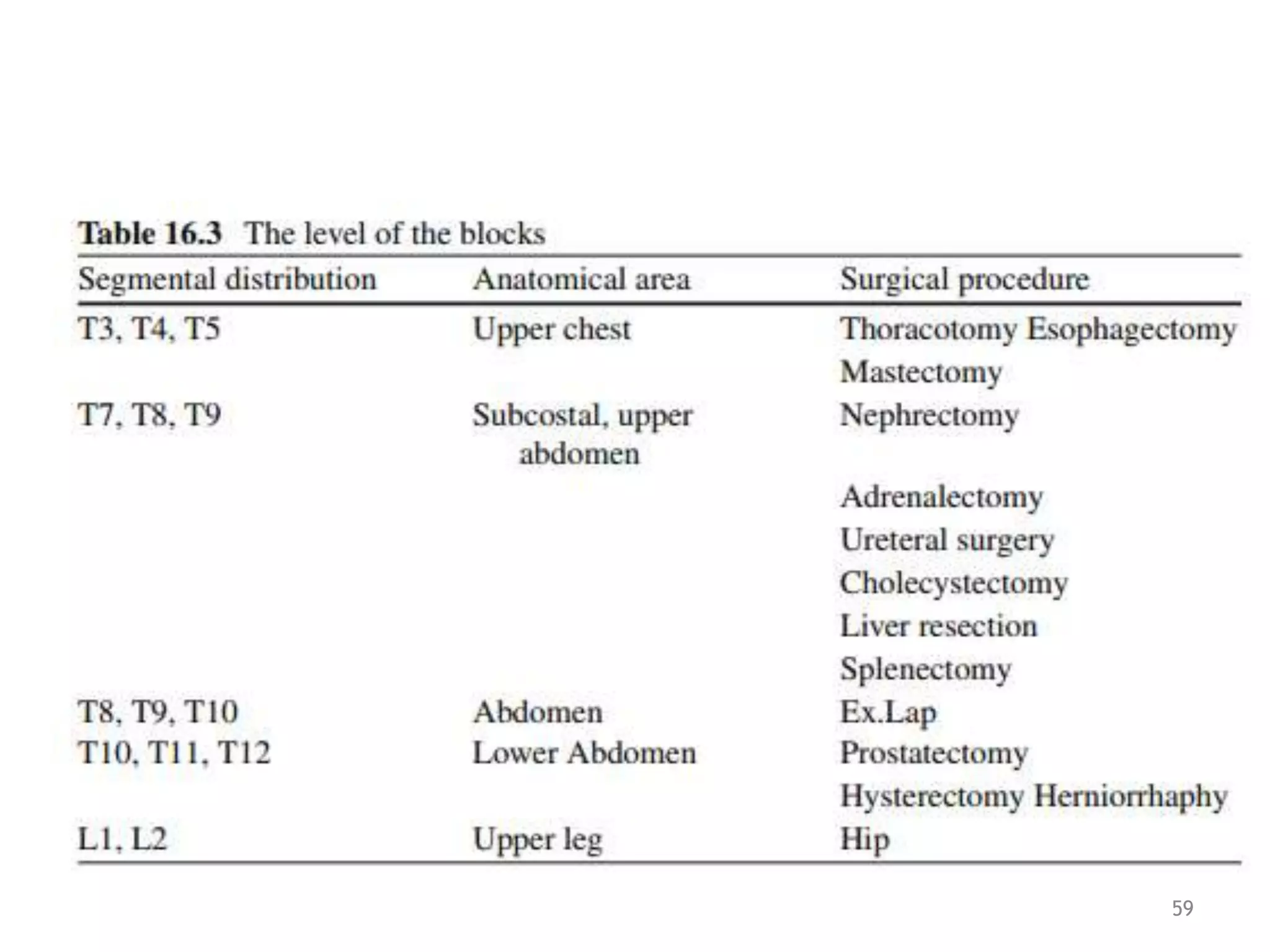
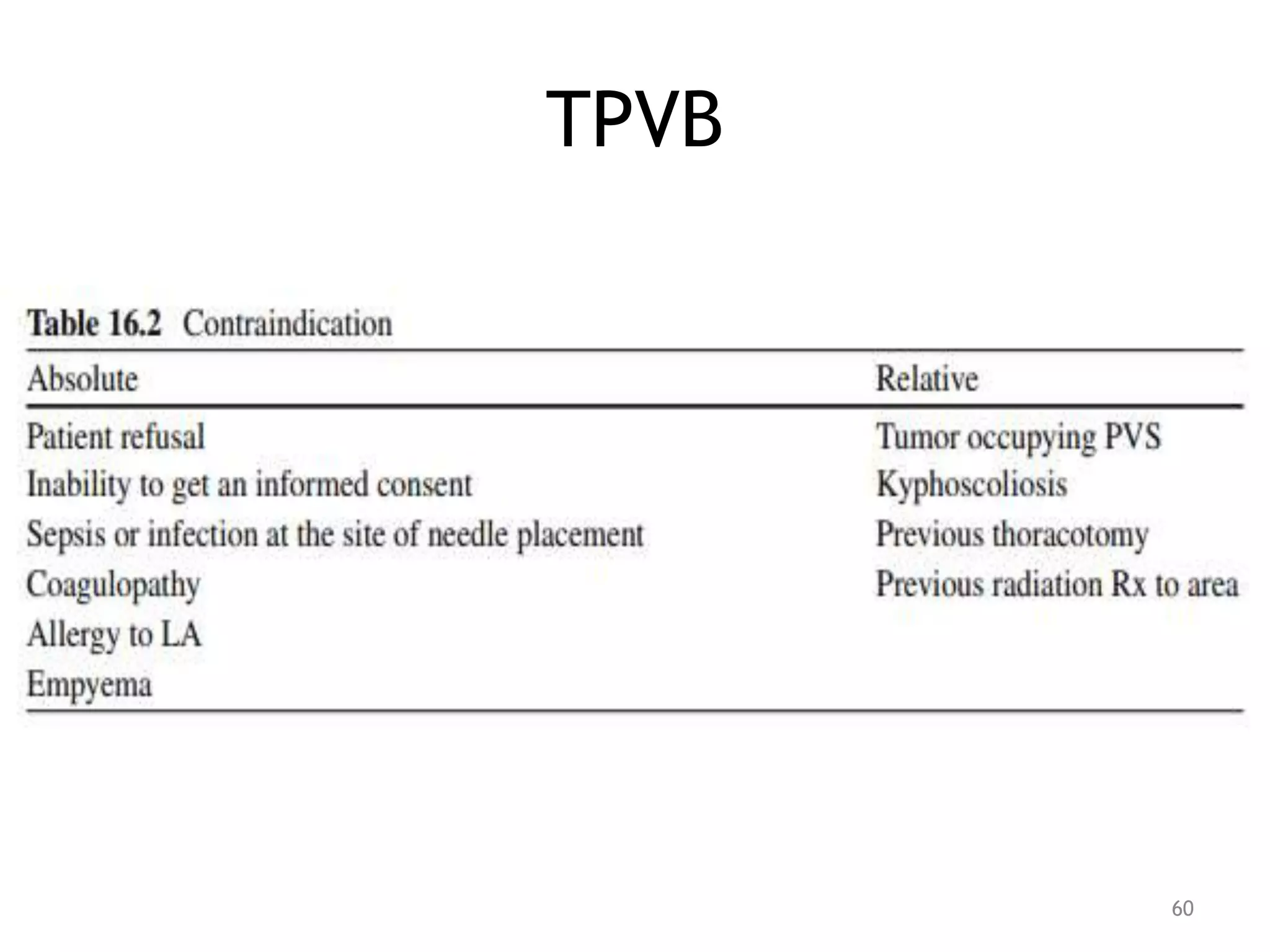
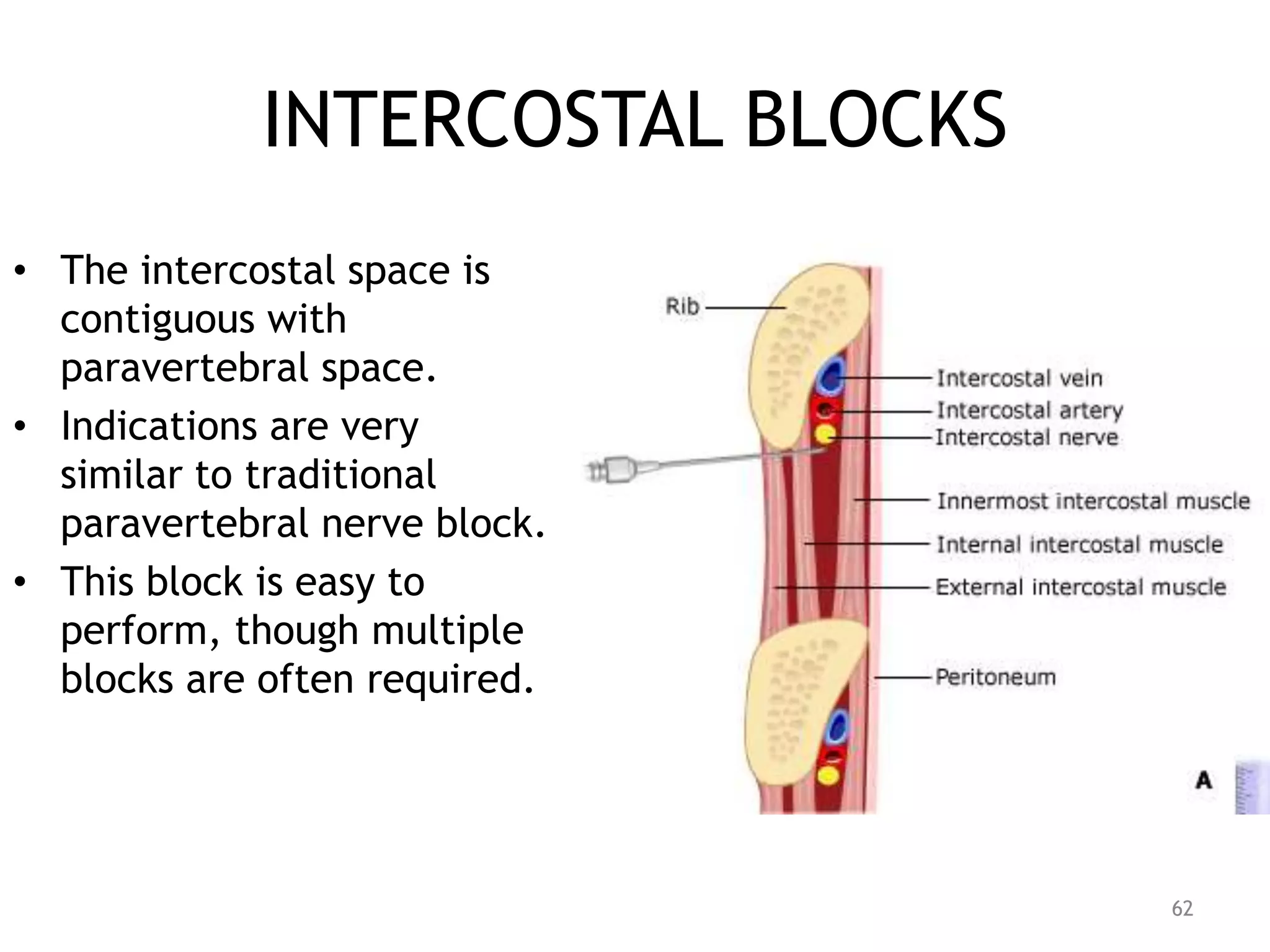
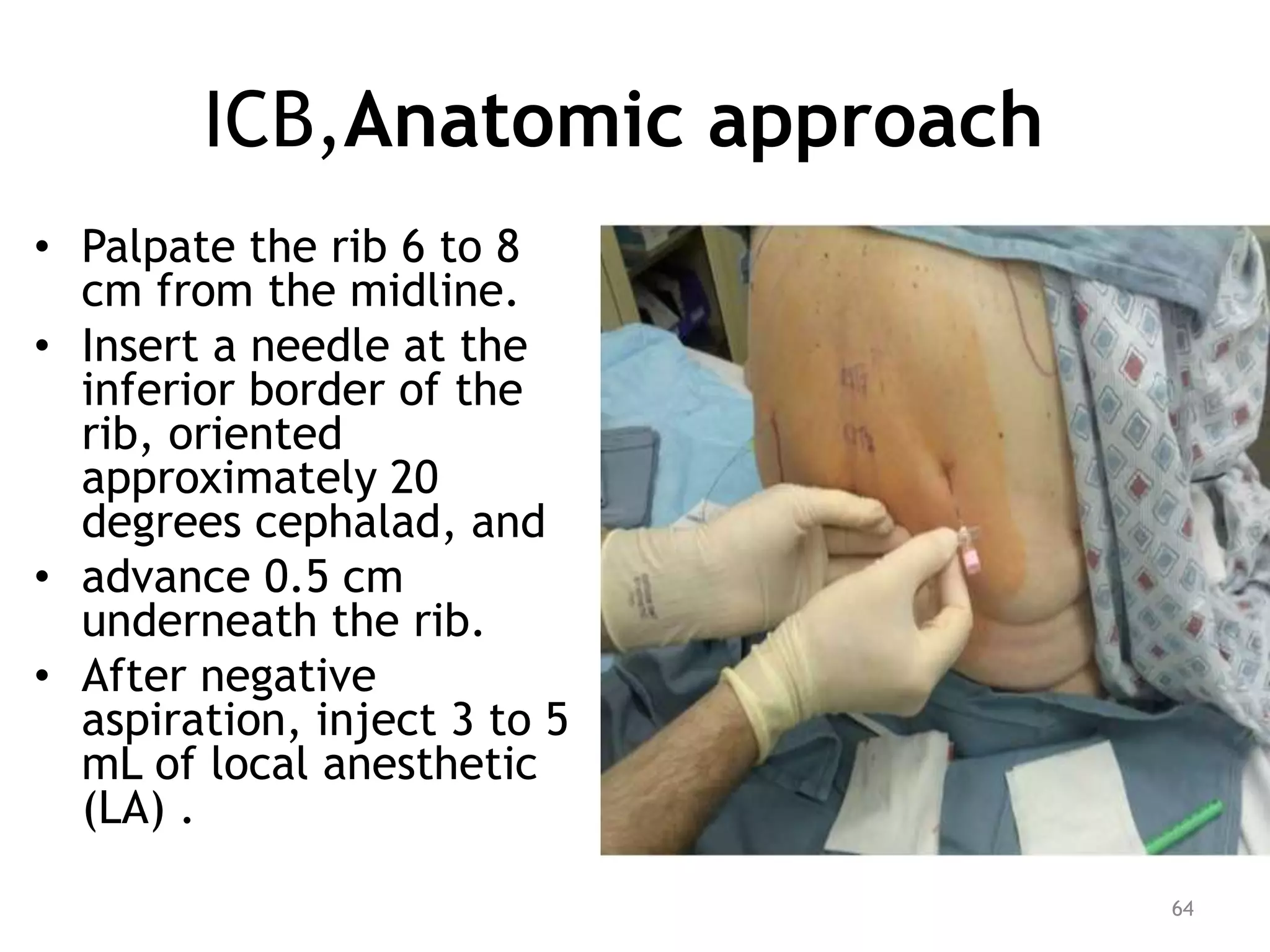
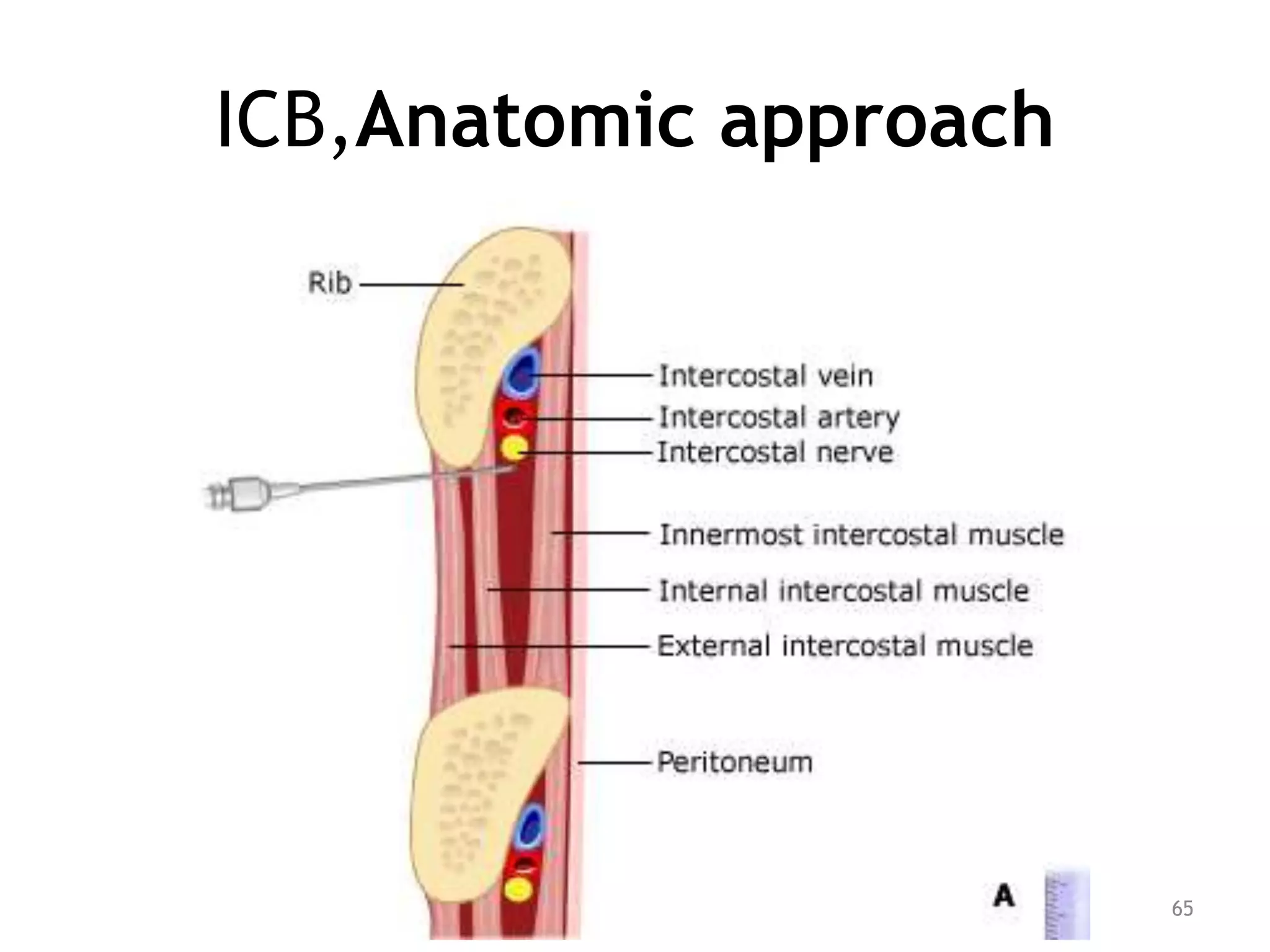
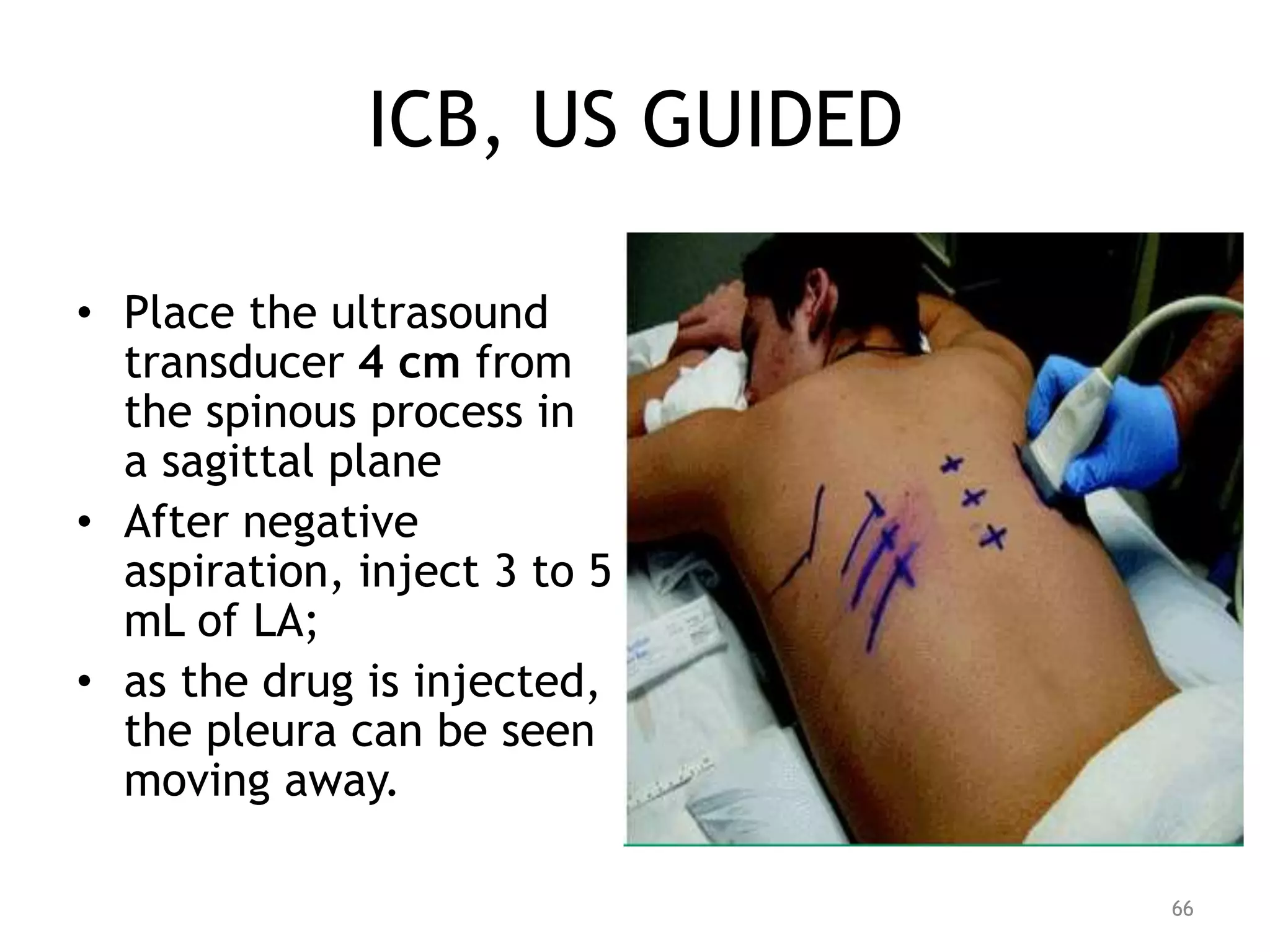
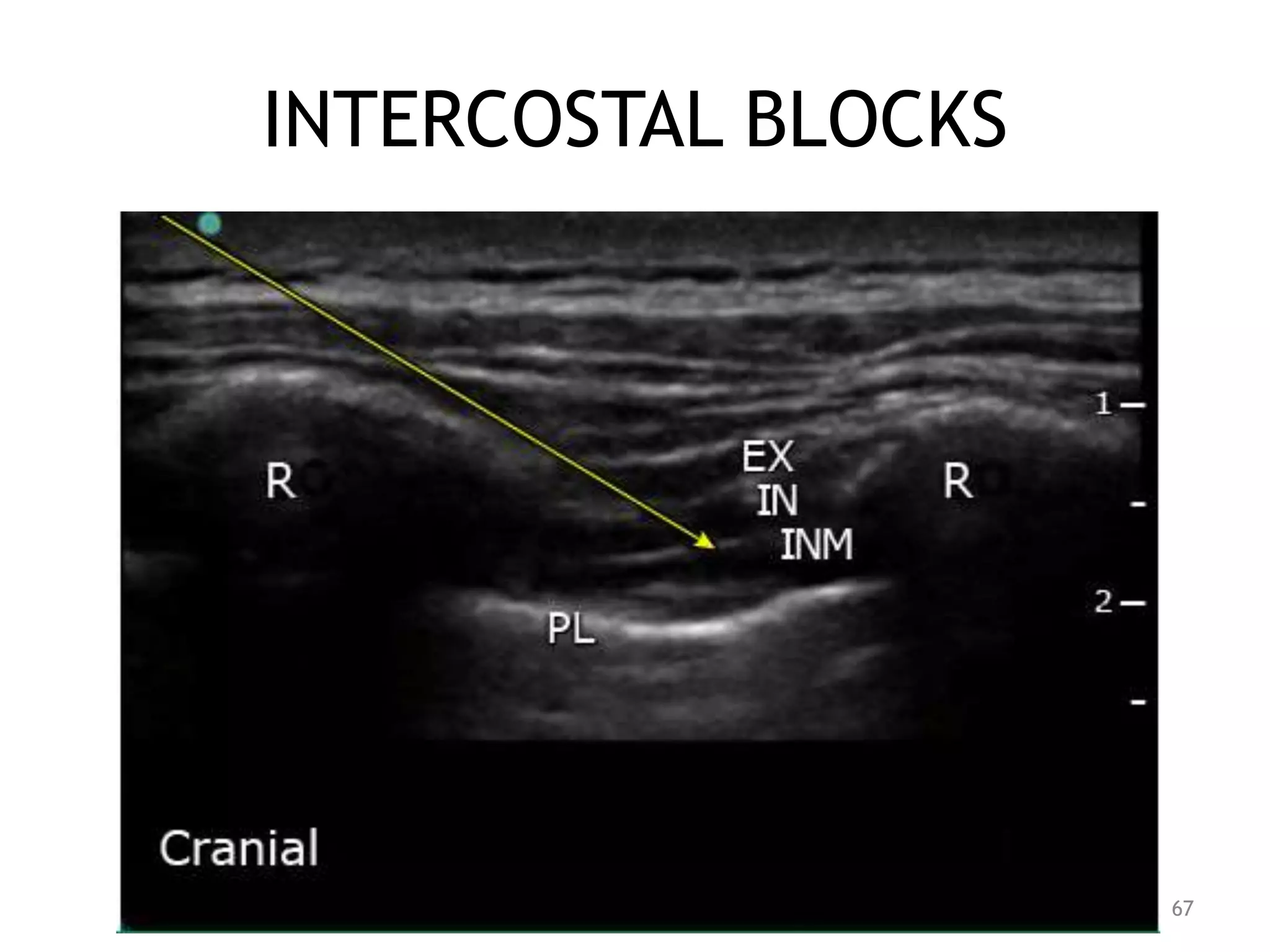
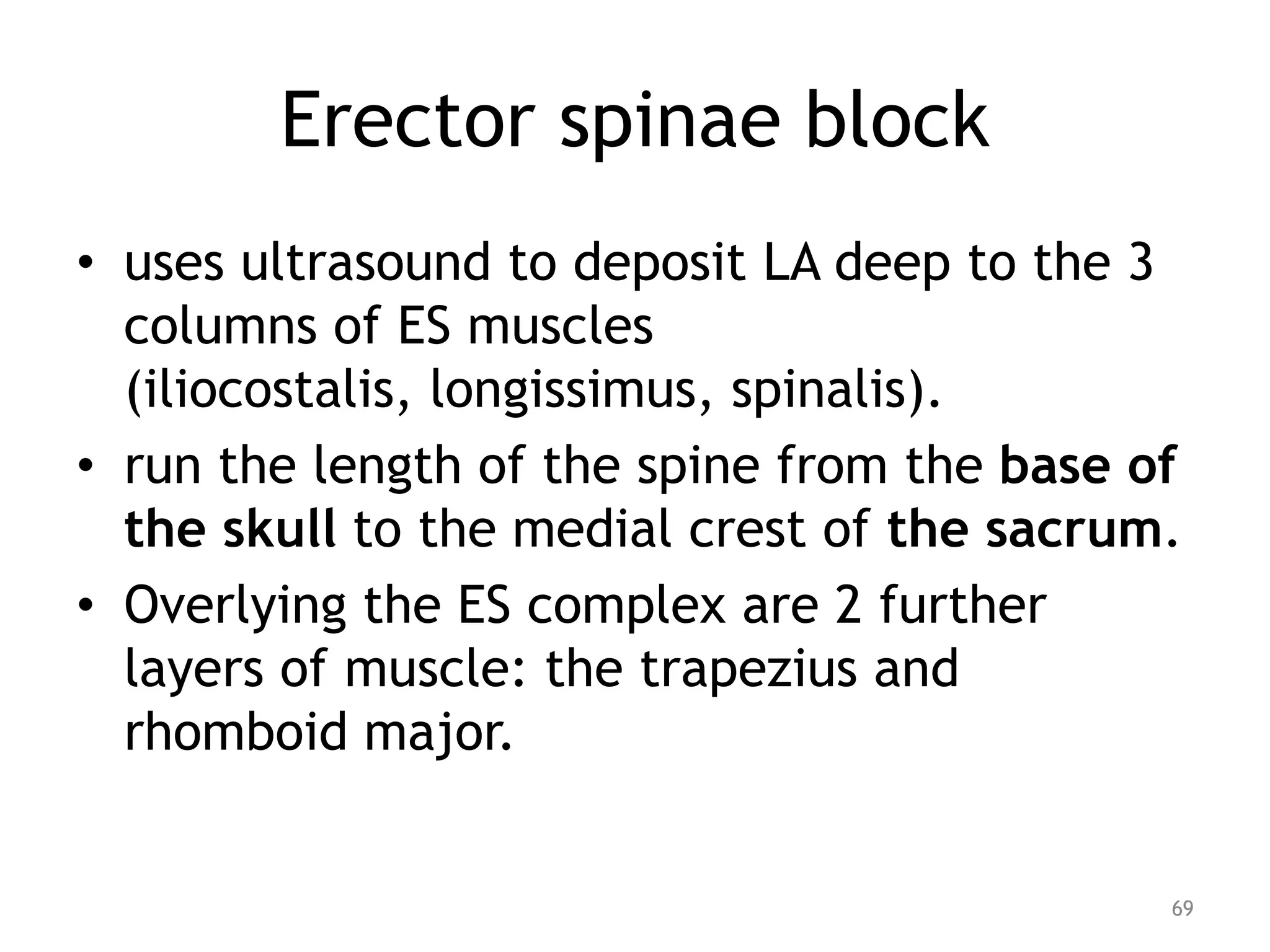
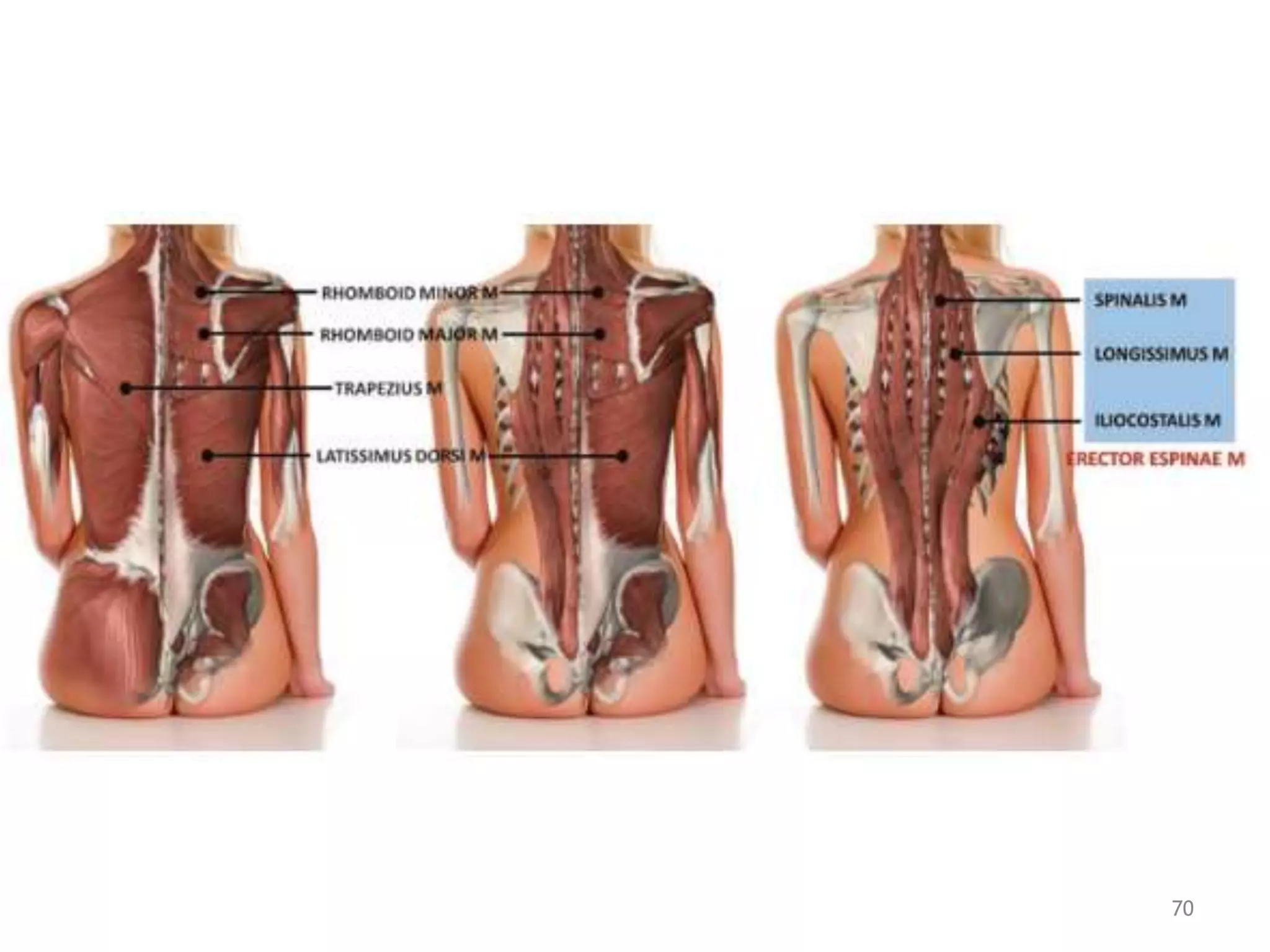
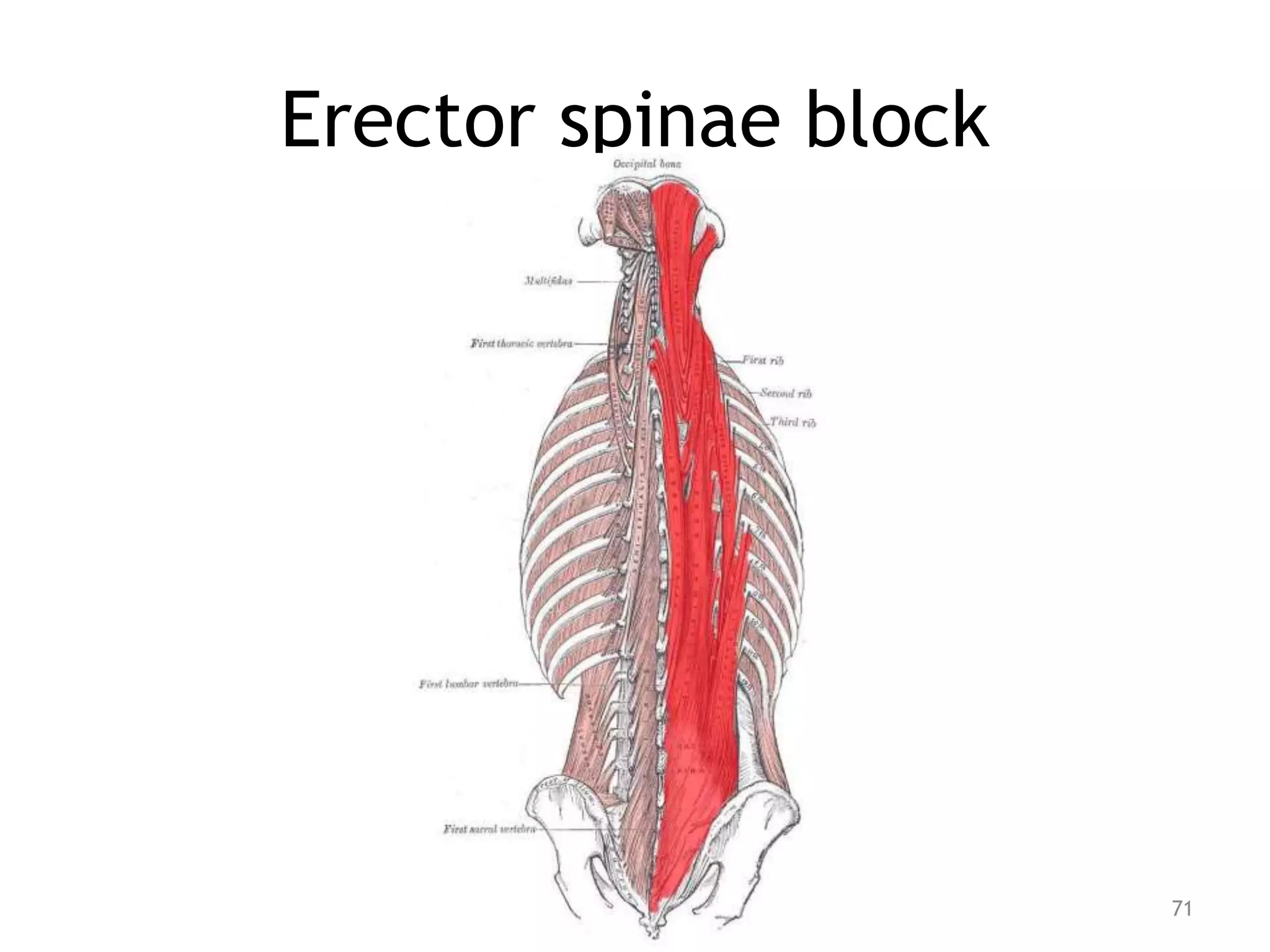
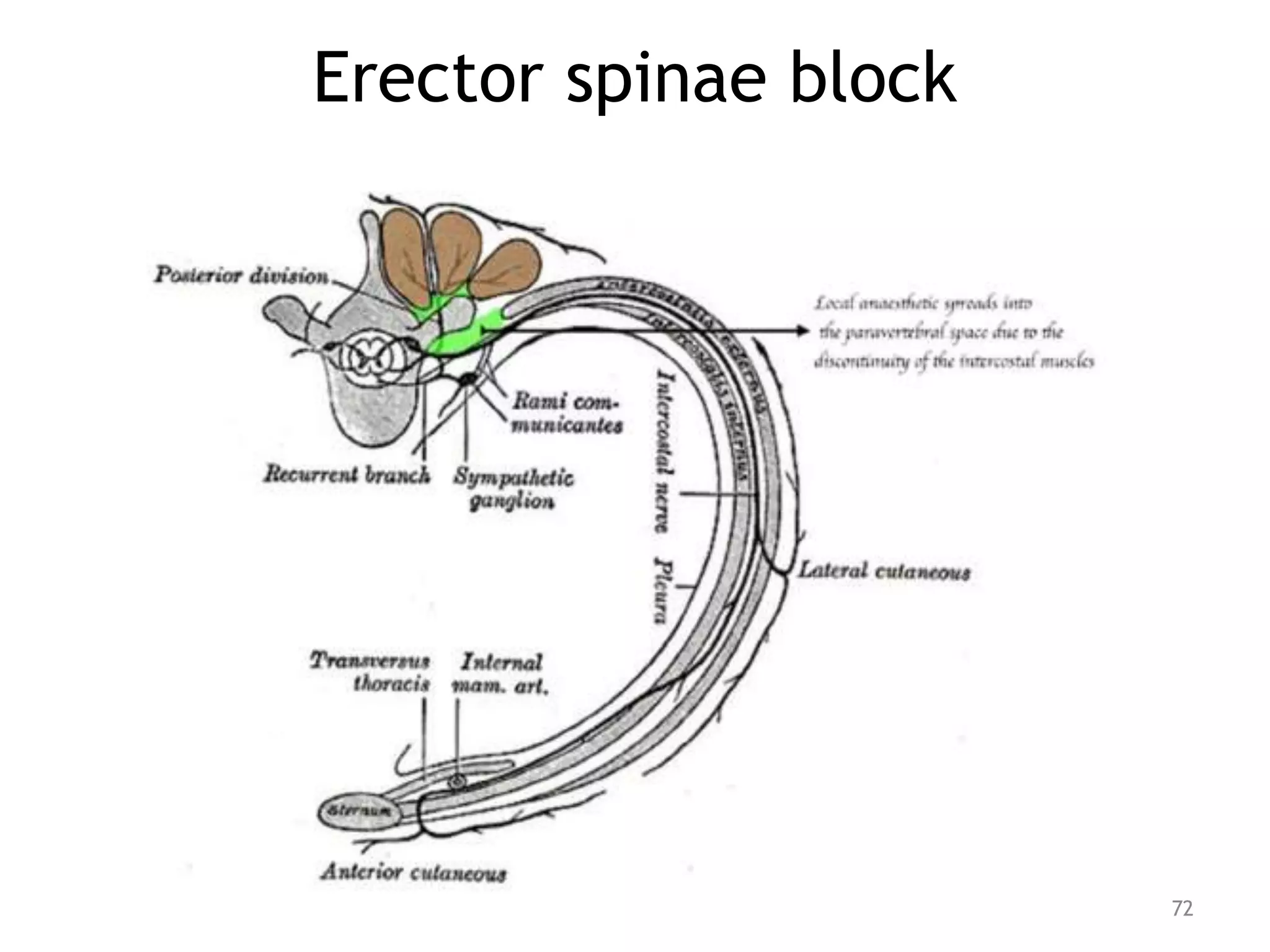
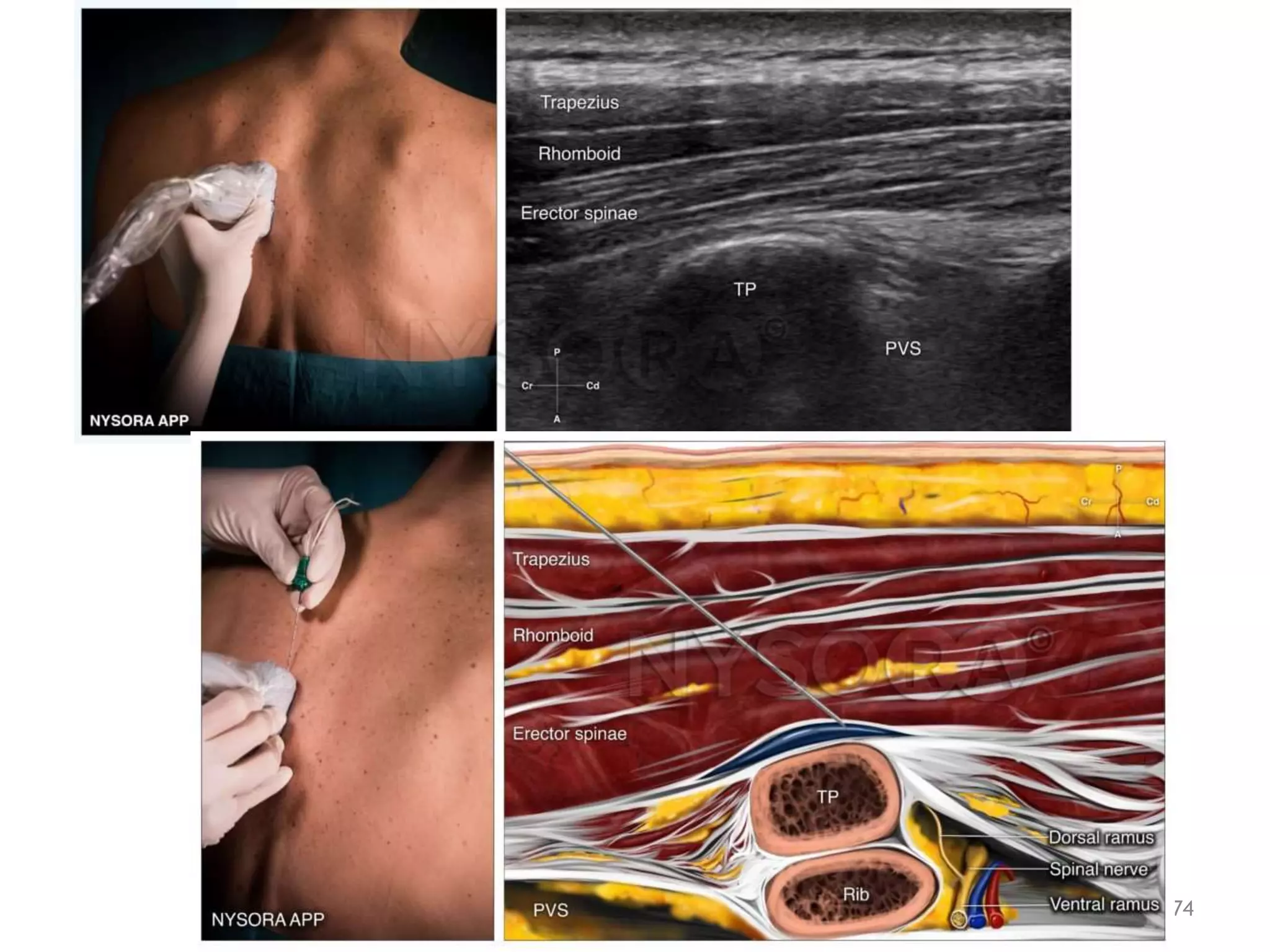
The seminar covered truncal blocks including abdominal wall blocks like transversus abdominis plane (TAP) block, rectus sheath block, and ilioinguinal/iliohypogastric nerve blocks as well as chest wall blocks such as serratus plane block, pectoral nerve blocks, thoracic paravertebral block, and intercostal blocks. Techniques like ultrasound-guided quadratus lumborum block and erector spinae block were also described along with relevant anatomy, indications, and potential complications of truncal blocks.